![]()
PART ONE
THEORY AND CONTEXT
![]()
1 STUDYING HEALTH POLICY
CHAPTER CONTENTS
- Introduction
- What is a ‘policy’?
- Defining the characteristics of public policy
- Scoping the field of health policy analysis
- Conceptual frameworks in the analysis of health policy
- ‘Power’ as a key concept for critical health policy analysis
INTRODUCTION
Where there was once a broad agreement about the main constituents of the study of health policy, many of these assumptions are today subject to dispute. In introducing the reader to the field of health policy studies, this chapter examines the divergent theoretical frameworks that are drawn upon in the contemporary analyses of policy and, in particular, the differences in the way in which political power is conceptualised.
WHAT IS A ‘POLICY’?
Policy as a concept is neither a specific, nor indeed a concrete phenomenon, so to attempt to define it poses a number of problems. It is more fruitful to see policy as a course of action or ‘web of decisions’ or decision network, rather than a single identifiable decision (Hill, 1997: 7). Policies are on-going and dynamic and therefore are subject to change, particularly in response to problems arising out of implementation of a decision. Policy can also be just as much about inaction (‘non-decision-making’) as action; the maintenance of the status quo. Policy can also be an outcome of actions taken over a period of time, by ‘low-level actors’ within an organisation, which have not been formally sanctioned by a decision taken by those at the ‘top level’. Here, policy can be seen as emerging as the outcome of a set of processes rather than as a formal decision to follow a course of action. It should also be noted that in the French language no distinction is made between the words ‘policy’ and ‘politics’. In this sense, a formal model of policy-making would be rejected in favour of an understanding of ‘policy’ as political in the widest sense of the word.
DEFINING THE CHARACTERISTICS OF PUBLIC POLICY
Is there then anything distinctive about public policy as against those policies adopted by corporate organisations or even those of individuals ? In terms of simple characteristics, the answer is ‘no’. However, because public or state policy emanates from the government as the legal authority within a society nation, it follows that it has a primacy and influence over all other policies (private and personal). These public policies provide the legalistic framework through which individuals must operate. A private company for example cannot decide that it wants to employ women at a lower rate of pay for performing a job than male employees doing the same job. This is because it would be in breach of the Equal Opportunities legislation and therefore subject to legal sanctions.
One possible starting point in attempting to define public policy and policy-making is to examine how the UK government itself has presented these issues. Relatively early on in its first term in office, the New Labour government published a White Paper entitled Modernising Government (Cabinet Office, 1999), which sets out the ‘official’ view of policy-making as follows: ‘Policy making is the process by which governments translate their political vision into programmes and actions to deliver “outcomes” – desired changes in the real world’ (Cabinet Office, 1999: para 2.1). The White Paper goes on to outline the six key characteristics associated with what it termed a ‘modernising’ (health, social, economic, etc.) policy; these characteristics are set out below:
- Strategic – A modernising policy looks ahead and contributes to long-term government goals.
- Outcome focused – A modernising policy aims to deliver desired changes in the real world.
- Joined up – A modernising policy operates across the organisational boundaries of government.
- Inclusive – A modernising policy is fair and takes account of the interests of all.
- Flexible and Innovative – A modernising policy tackles cause, not symptoms, and is not afraid of experimentation.
- Robust – A modernising policy stands the test of time and works in practice from the start.
This definition will be returned to again later within the book as one possible outcome measure of health policy, utilising the government’s own terms of reference.
SCOPING THE FIELD OF HEALTH POLICY ANALYSIS
The academic study of health policy in the UK has traditionally been focused upon the formal institutions of the welfare state charged with the treatment and care of the sick. The primary concern of these studies has been the analysis of the organisations and structure of the NHS, as well as the rather more poorly defined area of public health. From the late 1950s onwards, health and social policy studies as an academic discipline established a conceptual base, drawing almost exclusively upon its own internal theoretical and analytical frameworks, rooted in a set of implicit political and philosophical assumptions associated with the emergence and development of the post-war welfare state. This de facto delineation of the academic study of health policy effectively played down the potential contribution of the disciplines of sociology, politics and economics to policy analysis. However, over the last two decades this rather narrow approach to the subject has come under sustained criticism, largely as a consequence of real world political developments. The health and social policies of the Conservative governments of the late 1980s and early 1990s, and to a debatable extent those of the New Labour governments since 1997, have sustained the neo-liberal challenge to the very idea of universal state provision of social welfare and health services. Thus, the very basis of an academic discipline centred on the welfare state was itself disrupted. It was now no longer appropriate or relevant to study social and health policy in isolation from other forms of social organisation and social structures (Coffey, 2004: 3).
The work of many of the early pioneers of health and social policy analysis in Britain, such as that of Richard Titmuss (1958, 1970), Peter Townsend (1970a), and Brian Abel-Smith (Abel-Smith and Townsend, 1966), was informed by a detailed sociological analysis of the workings of the welfare state and its impact on the health and social welfare services on the lives of ordinary people. These studies revealed that the health and welfare needs of many of the most deprived groups in post-war Britain were not being met because the state left the forces of the market economy largely unchecked. These structures of exploitation were seen to reproduce poverty across the generations and to sustain poor levels of health. The criticisms levelled at the academic discipline of health and social policy analysis in the 1980s and 1990s were that it chose to focus on organisational matters whilst all too often it neglected to assess whether the founding social and political goals of the welfare state (including the NHS) were still relevant to the health and social needs of the population – for example, whether the worst effects of poverty and low income were being addressed, or whether access to good quality healthcare was available to all irrespective of social status and income. These were the original concerns that inspired the work of Titmuss, Townsend and Abel-Smith, who, whilst supportive of the goals of the welfare state, always engaged in a critical analysis of the practice of the NHS and other state welfare institutions.
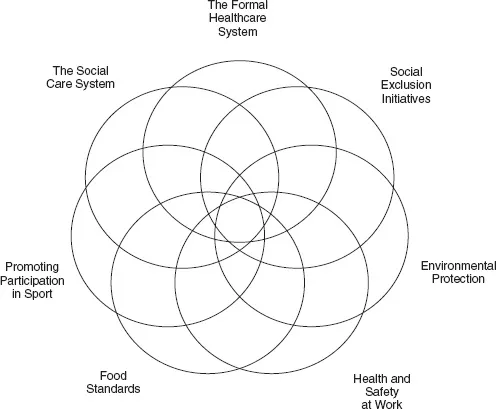
As will be apparent from the discussion in the introductory chapter, the aim of this book is to engage in a process of critical analysis of contemporary health policy. The first stage in this process, given the previous discussion concerning the limitations of traditional analytical approaches, is to delineate in its widest sense the potential field of health policy analysis. This means moving beyond the confines of an analysis of the formal institutions of healthcare, and assessing all those policies (both public and private) that impact upon health and well-being of the population, employing the conceptual tools of both sociology and political science; this scope of policy analysis is set out in Figure 1.1.
THE FORMAL HEALTHCARE SYSTEM
This was gradually constructed over the course of a century-and-a-half in order to better manage the clinical needs of those in the population who were sick and disabled, and this largely remains its focus to this day. The healthcare system in Britain has historically never given priority to disease prevention and health promotion. Apart from policies directly affecting the formal healthcare system itself, also included in Figure 1.1 are the following areas with potential impacts on the health outcomes of the population, and which therefore should be a concern of health policy analysis.
ENVIRONMENTAL PROTECTION
This covers areas such as atmospheric pollution, the use of toxic chemicals and radiation, the effects of global warming, the use of non-renewable resources, the planting of genetically modified (GM) crops, and many other developments with the potential to compromise the natural environment and therefore negatively affect the long-term health of the population. Policies include the attempt to reduce carbon emissions, the promotion of renewable energy sources and recycling, and the safeguarding of individuals from the effects of poor air quality.
Figure 1.1 Scoping the field of health policy analysis
FOOD STANDARDS
This is the area of state regulation and enforcement of legislation which serves to protect the public’s health and consumer interests in relation to food. This covers issues of food hygiene, nutritional standards, and food labelling.
HEALTH AND SAFETY AT WORK
The Health and Safety Commission (HSC) and the Health and Safety Executive (HSE) are responsible for the enforcement of legislation and the regulation of almost all the risks to health and safety arising from work activity in Britain, as well as many other aspects of the protection both of workers and the public.
SOCIAL CARE SYSTEM
This covers those aspects of care provided or purchased by local authorities outside the formal healthcare system for those living with chronic illness and disability, learning and physical disabilities, as well as those with long-term mental health problems.
SOCIAL EXCLUSION INITIATIVES
This covers those government intervention programmes that have been introduced over the past decade in order to remove families from living in poverty, with all its negative impact on long-term health. These initiatives include the Sure Start programme, designed to improve the health and emotional development for young children living in deprived communities by increasing the availability of childcare for all children and supporting parents in their aspirations towards employment. Britain also has the highest rate of teenage pregnancy of any Western European country. This ‘social problem’ is seen to reflect low expectations as well as economic deprivation, and as such is recognised as having long-term health and social implications for both the young mothers and their children; a nationally coordinated action plan now aims to reduce this high rate.
PROMOTING PARTICIPATION IN SPORT
It has become a truism that the popularity of sport in Britain is restricted to watching it rather than active participation. Sport England (formerly the English Sports Council) is the body responsible for distributing funds and providing strategic guidance for promoting sporting activity in England. Its slogan is ‘Get active, healthy and happy’, which emphasises the importance of sport participation for the health of a largely sedentary population. The funding for this organisation comes from central government and the National Lottery, and since 1994, it has invested over £2bn of Lottery funds and £300 million from the Treasury into supporting not only professional sport but in promoting greater community participation in sport in England. However, with the awarding of the 2012 Olympic Games to London, the debate about whether disproportionate amounts of public money is spent on elite rather than grassroots sport has widened.
All those areas where policy impacts upon health outcome will be explored in the book, although the substantive focus will be upon the formal healthcare system. However, the analysis will not be restricted to an examination of White Papers, strategy documents and the top-down interventions by the Department of Health. A significant concern of this textbook is how these centrally devised policies are interpreted and implemented in practice.
CONCEPTUAL FRAMEWORKS IN THE ANALYSIS OF HEALTH POLICY
Having delineated the field of health policy analysis the next stage is to critically examine the range of conceptual frameworks that are used to assess health policy.
All academic and indeed all so-called common-sense understanding, whether practical or theoretical, involves the use of some sort of model or conceptual schema in order to simplify and make sense of the tremendous variety of potential variables that exist in the social and physical world. In the complex process of health policy formation and implementation within a dynamic political and economic system such as exists within the UK, the application of conceptual frameworks is essential if we are to gain an understanding of the hows and whys of current health policy. These frameworks are drawn from a variety of often conflicting theoretical perspectives. For example, the analysis of the institutions and organisational processes associated with the modern welfare state has traditionally been heavily reliant upon models which derive from a theorisation of the historical role of the State as vehicle for the social and national transformation and development. However, this is just one theorisation of the role of the State within modern capitalist societies, there are many other competing explanations of the role of the State that can be found within sociological analysis; these are discussed in detail in Chapter 2.
As discussed in the Introduction, the aim of this textbook is to contextualise the essentially political process of formulating and implementing health policy by locating specific developments within a broader set of social and institutional processes. This involves synthesising theoretical constructs relevant to the analysis with an empirical description of the specific processes associated with the development of a particular policy. This is what is meant by integrating theory with practice. Hence, while the opening chapters of the book give broad descriptions of the range of theoretical frameworks utilized within policy analysis, this should not be seen as a process of ‘front-loading’. Where they are most relevant to the discussion of specific health policy developments, ‘key concepts’ deriving from a wide range of theoretical traditions within sociology and political theory will be introduced to facilitate analysis. This approach is...