![]()
SECTION V
Diagnosis and Management
![]()
Chapter 10
AN APPROACH TO THE DIAGNOSIS OF CYANOTIC NEONATE FOR THE PRIMARY CARE PROVIDER
P. SYAMASUNDAR RAO, MD
Introduction
Newborn infants with distress caused by heart defects may not live unless they are treated correctly and quickly.1–4 Cyanosis is a crucial manifestation of congenital heart defects (CHDs) in the neonate. Pediatric cardiology consultation and/or an echocardiographic study may assist in making a diagnosis. However, such services may not be readily accessible to all newborn babies. An appreciation of the problems related to cyanotic infants by the primary care physician, whether he/she is a pediatrician or a neonatologist, may be useful. At the outset, it should be emphasized that (1) complex physiological and anatomical alterations take place during and immediately after birth5–7; (2) severe cyanotic CHD can exist without a cardiac murmur; (3) a loud murmur does not automatically suggest that the reason for the distress in the baby is related to a heart defect; (4) when a murmur is detected, it is not necessarily characteristic for a specified CHD; and (5) lack of cardiomegaly on a chest x-ray image does not eliminate severe CHD.
In this chapter, the author will name the causes of cyanosis in the newborn infant; delineate techniques to distinguish cardiac from noncardiac causes of cyanosis; and describe an approach to formulate a cardiac diagnosis prior to echocardiographic and Doppler studies.
Causes of Neonatal Cyanosis
The etiology of cyanosis may chiefly be categorized into respiratory, cardiac and central nervous system (CNS) disorders, persistent pulmonary hypertension (PPHN), and a miscellaneous group of abnormalities and are listed in Table 10.1.
Table 10.1. Causes of cyanosis
- Respiratory disorders
- Cyanotic heart defects
- Persistent fetal circulation
- CNS disorders
- Miscellaneous
|
The respiratory disorders may be subgrouped as pulmonary parenchymal disorders and diseases causing mechanical interference with lung function, and are shown in Table 10.2.
Table 10.2. Respiratory disorders causing cyanosis
| A. Pulmonary parenchymal diseases - Hyaline membrane disease
- Aspiration syndrome
- Pneumonia
- Rare disorders like pulmonary hemorrhage or Wilson–Mikety syndrome
B. Diseases causing mechanical interference with lung function - Diaphragmatic hernia
- Pneumothorax and pneumomediastinum
- Tracheo-esophageal fistula
- Lobar emphysema
|
The cyanotic CHD may be subdivided into 3 groups, depending upon pulmonary vascular markings on a chest x-ray (Table 10.3). PPHN (also referred to as persistent fetal circulation [PFC]) is an important cause of cyanosis; this is because of associated right-to-left shunt across the patent foramen ovale (PFO) and/or patent ductus arteriosus (PDA).
Table 10.3. Heart defects causing cyanosis
| A. Decreased pulmonary vascular markings - TOF
- Pulmonary atresia (stenosis) with intact ventricular septum
- Tricuspid atresia
- Complex PS
B. Increased pulmonary vascular markings - TGA
- HLHS
- CoA syndrome
- Multiple left-to-right shunts
C. Severe pulmonary venous congestion - TAPVC (infradiaphragmatic type)
- HLHS (with intact atrial septum)
- Severe CoA
|
CNS disorders, which are likely to cause cyanosis, are shown in Table 10.4; the cyanosis as a rule is related on hypoventilation.
Table 10.4. CNS disorders causing cyanosis
- Intracranial hemorrhage
- Intracerebral malformations
- Severe intracranial infections
- Primary seizure disorders
|
A remarkable group of miscellaneous disorders, which may cause cyanosis, are listed in Table 10.5.
Table 10.5. Miscellaneous disorders causing cyanosis
- Polycythemia
- Hypoglycemia
- Methemoglobinemia
- Shock and sepsis
- Maternal drugs
|
Cardiac versus Noncardiac
A diagnosis of the cause of the cyanosis (see Tables 10.1–10.5) can frequently be accomplished by the use of usual clinical evaluation and laboratory studies. Respiratory causes may be assumed if there were complications during pregnancy and/or delivery, fever in the mother before birth, onset of cyanosis within the first few hours following birth, prematurity, inappropriate weight for gestational age, asphyxia neonatorum, meconium staining, and/or low Apgar score. Chest x-ray will more often than not aid in recognizing respiratory problems caused by lung parenchymal disease and those that produce mechanical interference with lung function (see Table 10.2). Arterial blood gas examination is helpful in distinguishing cardiac from lung diseases. The PaCO2 is increased in pulmonary disorders, but not consistently so in CHDs. Nevertheless, there are some babies in whom it is not easy to distinguish between severe pulmonary disease (PD) and cyanotic CHD.
Improvement in arterial PO2 following 100% oxygen administration in an oxyhood for a period of 15 minutes1,9 is helpful in the differential diagnosis; significant increase in the PO2 occurs in infants with PD while no noteworthy increase in PO2 (< 10 torr) is seen in cyanotic CHD babies. A PaO2 >150 torr is extremely suggestive of pulmonary problem. A higher PO2 in the right radial artery blood sample than that in the umbilical artery sample is suggestive of right-to-left shunt via the ductus arteriosus (DA). This may be secondary either to PPHN or to obstruction of aortic arch (eg, interrupted aortic arch [IAA] and severe aortic coarctation).
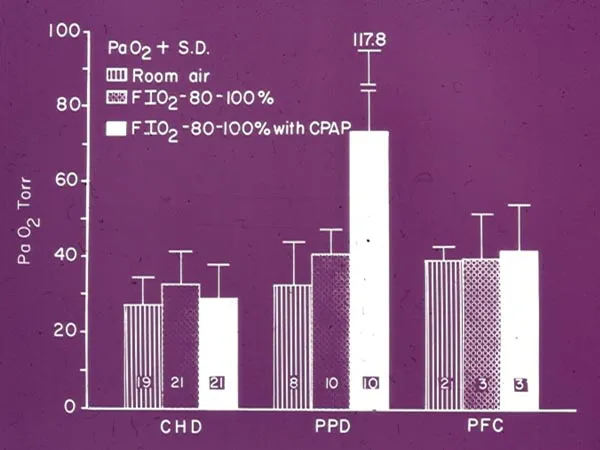
Although failure to increase PO2 with 100% O2 is greatly indicative of cyanotic CHD, some neonates with severe PD do not demonstrate elevation in PO2. In such babies, continuous positive airway pressure (CPAP) may be useful in the differentiation of pulmonary from heart disease (Figures 10.1). Application of 8 to 10 cm H2O CPAP with 100% O2 for a period of 10 to 15 minutes via a face mask is likely to show improvement in PO2 (> 10 torr) in babies with PD, whereas no change or a decrease may be seen in cyanotic CHD infants.10,11
Figure 10.1. Bar graph demonstrating usefulness of CPAP in the diagnosis of cyanotic infants. In the congenital heart disease (CHD) and PFC groups, there was no increase in arterial PO2 following administration of 100% oxygen along with CPAP. In the PD group, while there was no increase in PO2 after 100% O2, the PO2 increased with CPAP. The PO2s are shown as mean + SD. The number of infants studies in each group is marked within bar. The data are derived from Reference 11.
Diagnosis of Specific Type of CHD
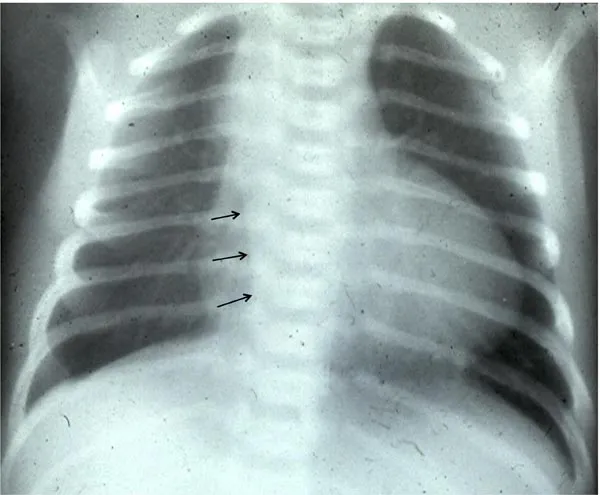
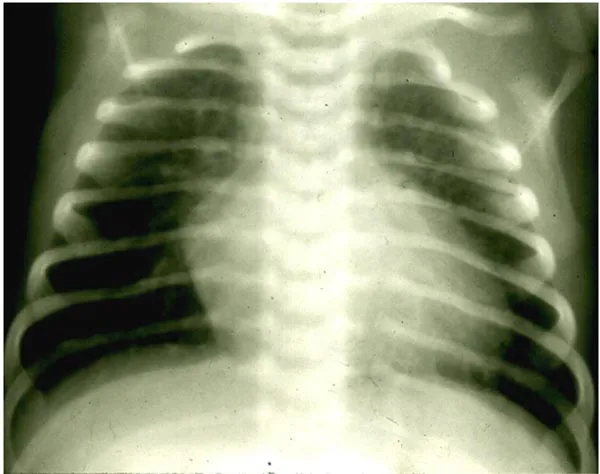
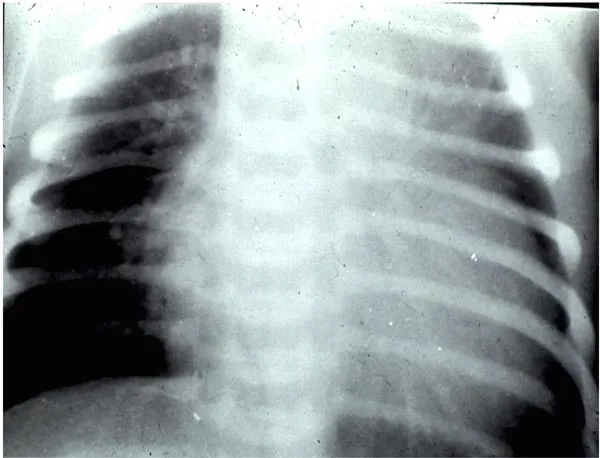
Having recognized a baby with a cardiac problem, additional designation of type of CHD is based on scrutiny of pulmonary blood flow (PBF) on a posterior–anterior view of a chest x-ray: (1) decreased pulmonary vascular markings (Figure 10.2); (2) increased pulmonary vascular markings (Figures 10.3 and 10.4); and (3) severe pulmonary venous congestion (Figure 10.5). High-quality chest x-ray with deep inspiration and without patient rotation is obligatory to accomplish precise evaluation of pulmonary vascular markings.
Figure 10.2. Chest x-ray of an infant with decreased PBF. Mild enlargement of the heart with markedly decreased PBF may be seen. Note right aortic arch (small arrows), which suggests that the diagnosis is likely to be TOF.
Figure 10.3. Chest x-ray of an infant with increased PBF. Mild enlargement of the heart with moderately increased PBF is seen. On further studies, this infant was demonstrated to have TGA with intact ventricular septum.
Figure 10.4. Chest x-ray of an infant with increased PBF. Severe enlargement of the heart with markedly increased PBF is seen. On further studies, this infant was diagnosed to have HLHS.
Figure 10.5. Chest x-ray of an infant with pulmonary venous congestion. A picture of severe pulmonary venous congestion with no significant enlargement of the heart is seen.
Decreased Pulmonary Vascular Markings
The most frequently encountered CHDs in this group are shown in Table 10.3. Diagnosis of infants with decreased PBF can be made by analysis of the ECG (Figure 10.6). Advanced knowledge of ECG interpretation/understanding is not needed for this approach. Calculation of axis (mean frontal plane vector), which is learned in medical school, is su...