
eBook - ePub
Liver Transplantation
State of the Art
Abhinav Humar, Amit Tevar, Christopher Hughes
This is a test
Buch teilen
- 392 Seiten
- English
- ePUB (handyfreundlich)
- Über iOS und Android verfügbar
eBook - ePub
Liver Transplantation
State of the Art
Abhinav Humar, Amit Tevar, Christopher Hughes
Angaben zum Buch
Buchvorschau
Inhaltsverzeichnis
Quellenangaben
Über dieses Buch
The field of liver transplantation has undergone tremendous change and continues to evolve at a fast pace. This book covers topics beyond standard care and discusses issues that are new and rapidly evolving in the field. These include innovative surgical methods to maximize the donor pool, non-surgical methods to expand the existing pool of additional donors, the changing face of liver rejection, and management of infections in the presence of new antivirals.
This book is an interesting read for surgeons, hepatologists, and healthcare workers looking after patients who need or have had a liver transplant.
Contents:
- Preface
- Liver Transplantation for HCC: Moving Beyond Milan (Amit D Tevar)
- Liver Transplantation for Non-HCC Malignancies: Cholangiocarcinoma, Neuroendocrine Tumors, HEHE, and Colorectal Metastases (Daniel Zamora-Valdes and Julie K Heimbach)
- Developments in Donation After Cardiac Death in Liver Transplantation (David P Foley and David J Reich)
- Machine Preservation of Livers for Transplantation (Paulo Fontes, Arjan van der Plaats, Roberto Lopez, Kyle Soltys, Wallis Marsh, Ruy Cruz, Banan Babak, William R Light, and Christopher Hughes)
- Living Donor Hepatectomy: Laparaoscopic and Robotic Techniques (Salvatore Gruttadauria, Giovanni B Vizzini, Duilio Pagano, Bruno G Gridelli, and Angelo Luca)
- Adult Living-Donor Liver Transplant: Right Lobe (Young-In Yoon and Dong-Sik Kim)
- Adult Living-Donor Liver Transplant: Left Lobe (Hillary J Braun, Garrett R Roll, and John Paul Roberts)
- Pediatric Liver Transplantation with Technical Variant Allografts (Kyle Soltys, Geoff Bond, Rakesh Sindhi, and George Mazariegos)
- ABO-Incompatible Liver Transplant (Abhideep Chaudhary, Prashant Pandey, and Sunil Taneja)
- New Trends in Immunosuppression for Liver Transplantation: Minimization, Avoidance and Withdrawal (Shoko Kimura, Fermin Fontan, and James F Markmann)
- Antibody-Mediation Rejection in Liver Transplantation (James F Trotter)
- Hepatitis C and Liver Transplantation in the Era of New Antiviral Treatments (Elizabeth C Verna and Robert S Brown Jr)
- Obesity in Liver Transplantation (Michele Molinari and Subhashini Ayloo)
- Liver Transplantation for Metabolic Disease (Patrick McKiernan and Kyle Soltys)
- Fulminant Hepatic Failure: Integrating Devices with Liver Transplantation (Nigel Heaton and Shirin Elizabeth Khorsandi)
- Future Directions in Liver Replacement Therapy: Liver Xenotransplantation (Burcin Ekser and David K C Cooper)
Readership: Hepatologists, and surgeons and nurses in hepatology.
Key Features:
- Covers topics that are new and rapidly evolving in liver transplantation
- Written by experts in liver transplantation
Häufig gestellte Fragen
Wie kann ich mein Abo kündigen?
Gehe einfach zum Kontobereich in den Einstellungen und klicke auf „Abo kündigen“ – ganz einfach. Nachdem du gekündigt hast, bleibt deine Mitgliedschaft für den verbleibenden Abozeitraum, den du bereits bezahlt hast, aktiv. Mehr Informationen hier.
(Wie) Kann ich Bücher herunterladen?
Derzeit stehen all unsere auf Mobilgeräte reagierenden ePub-Bücher zum Download über die App zur Verfügung. Die meisten unserer PDFs stehen ebenfalls zum Download bereit; wir arbeiten daran, auch die übrigen PDFs zum Download anzubieten, bei denen dies aktuell noch nicht möglich ist. Weitere Informationen hier.
Welcher Unterschied besteht bei den Preisen zwischen den Aboplänen?
Mit beiden Aboplänen erhältst du vollen Zugang zur Bibliothek und allen Funktionen von Perlego. Die einzigen Unterschiede bestehen im Preis und dem Abozeitraum: Mit dem Jahresabo sparst du auf 12 Monate gerechnet im Vergleich zum Monatsabo rund 30 %.
Was ist Perlego?
Wir sind ein Online-Abodienst für Lehrbücher, bei dem du für weniger als den Preis eines einzelnen Buches pro Monat Zugang zu einer ganzen Online-Bibliothek erhältst. Mit über 1 Million Büchern zu über 1.000 verschiedenen Themen haben wir bestimmt alles, was du brauchst! Weitere Informationen hier.
Unterstützt Perlego Text-zu-Sprache?
Achte auf das Symbol zum Vorlesen in deinem nächsten Buch, um zu sehen, ob du es dir auch anhören kannst. Bei diesem Tool wird dir Text laut vorgelesen, wobei der Text beim Vorlesen auch grafisch hervorgehoben wird. Du kannst das Vorlesen jederzeit anhalten, beschleunigen und verlangsamen. Weitere Informationen hier.
Ist Liver Transplantation als Online-PDF/ePub verfügbar?
Ja, du hast Zugang zu Liver Transplantation von Abhinav Humar, Amit Tevar, Christopher Hughes im PDF- und/oder ePub-Format sowie zu anderen beliebten Büchern aus Medicina & Gastroenterología y hepatología. Aus unserem Katalog stehen dir über 1 Million Bücher zur Verfügung.
Information
Thema
Medicina1.Liver Transplantation for HCC: Moving Beyond Milan
Amit D. Tevar
Division of Transplantation Surgery, University of Pittsburgh, Pittsburgh, PA 15213, USA
1.Introduction
Hepatocellular carcinoma (HCC) remains one of the most common causes of cancer death in the world. The incidence of HCC in regions of the world with endemic hepatitis B and C infection is substantially higher than other areas [1, 2]. Worldwide, the incidence of HCC is the sixth most common diagnosis of cancer and the third cause of cancer death, with the highest incidence rates in Asia and Africa [3]. This is likely a conservative estimate as many HCC diagnosed patients and deaths remain unreported in areas without significant medical infrastructure and reporting mechanisms. There has been a sharp rise in the incidence of HCC in the United States from 1.4/100,000 from 1976 to 1980 to 2.4/100,000 from 1991 to 1995. During this time period, there was also a significant increase in the overall mortality from HCC, with a 41% increase in the mortality rate based on review of the Surveillance, Epidemiology and End Results (SEER) database [4]. More recently in the United States despite a plateau in the overall incidence, there have been further significant increases in the liver cancer mortality from HCC, between 2007 and 2010 (Figure 1). This increase in mortality was found to be localized to African Americans, Hispanics, and white males greater than 50 years of age [5, 6].
Surveillance for HCC has been implemented for cirrhotic and fibrotic patients based on the recommendations of multiple societies. The current guidelines from the American Association of the Study of Liver Diseases (AASLD) suggest that ultrasound examination at an interval of 6 months for screening (Figure 2) [7]. Several studies have demonstrated the utility of a single dynamic imaging modality which demonstrates arterial uptake followed by “washout” in the venous phase to be sensitive for the noninvasive diagnosis of early and late HCC lesions [8, 9].
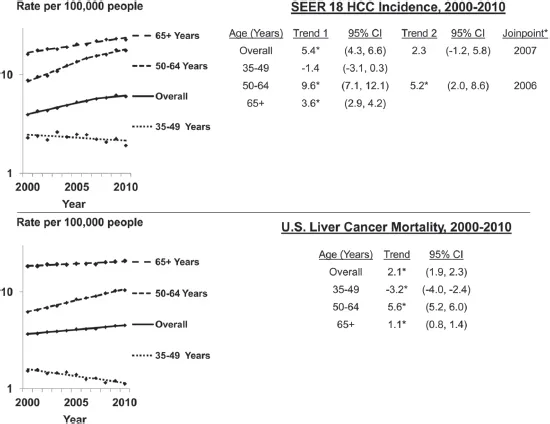
Figure 1.Age-adjusted SEER 18 HCC incidence and United States liver cancer mortality rates by age group and year, 2000–2010. CI: confidence interval; Trend: annual percent change (APC). Joinpoint regression defines when a trend changes. Up to one joinpoint is allowed in the 11-year period. (Reprinted with permission from Ref. [5]. Copyright © 2014 Nature Publishing Group.)
Note: * Slope of trend differs from zero (p < 0.05).
The staging of HCC remains a problematic and complex problem, as the disease progression and patient survival involves and changes with tumor biology, liver disease, and performance status. As a result, multiple staging algorithms have been proposed and attempted to be validated for prognosis of HCC. The first of these was introduced in 1985 as the OKUDA score and combined liver function and tumor parameters as predictor of survival [10]. The Italian Cancer of the Liver Italian Program (CLIP) reviewed 435 patients from 16 center and correlated survival based on liver function (Child–Pugh score) and tumor parameters, including portal vein thrombosis and alpha-fetoprotein (AFP) [11]. The Barcelona Clinic Liver Cancer (BCLC) system was introduced in 1999 and linked liver function, tumor parameters, and performance status into four stages: early, intermediate, advanced, and terminal [12]. The system of classification has been subsequently evaluated and validated in large Western and Asian cohorts with an enrollment of 3,892 Asian patients with HCC [13, 14]. Median survival times were noted to be 57.7 months at very early stage and 1.6 months at terminal stage. The BCLC is currently endorsed by European Associations for the Study of the Liver (EASL) and the AASLD and is used in practice throughout Europe and North America (Figure 3).
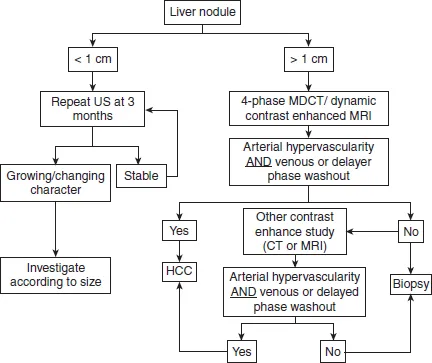
Figure 2.AASLD Practice Guidelines on HCC [7].
Several Asian scoring systems have also demonstrated significant survival prediction in the Asian cohort of patients. The Japan Integrated Staging (JIS) was originally released in 2003 and was based on a cohort of nearly 14,000 Japanese patients. Survival prediction is based on Japanese TNM factors (vascular invasion, number and size of lesions) and liver function (CPT Score) [16]. The survival accuracy was further increased in 2006 with the use of indocyanine green clearance on a review of 42,269 patients [17] and in 2008 included the addition of three separate HCC tumor markers and is now called the biomarker combined JIS (bm-JIS) [18]. Other Asian classification systems include the Hong Kong Liver Cancer (HKLC) classification system, the Taipei Integrated Scoring (TIS) system, the Advance Liver Cancer Prognostic System (ALCPS), the Chinese University Prognostic Index score, and others [19–22].
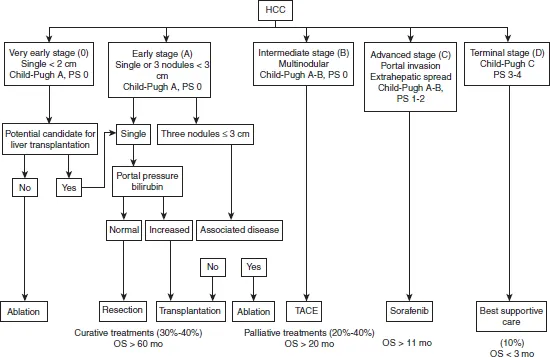
Figure 3.Barcelona Clinic Liver Cancer system. HCC: hepatocellular carcinoma; PS: performance status; TACE: transarterial chemoembolization. (Reprinted with permission from Ref. [15]. Copyright © 2016 The Author(s).)
2.Liver resection and local regional therapy as curative treatment options
Surgical resection as partial hepatectomy or hemihepatectomy is an effective modality of cure of the HCC in patients with noncirrhotic liver disease without evidence of significant portal hypertension. Approximately 80% of cases of HCC are found in patients with overt cirrhosis worldwide [23]. A very small cohort of patients exist in the East and West with noncirrhotic HCC and can be treated very effectively with primary surgical resection. A meta-analysis of all Eastern and Western studies on noncirrhotic HCC patients and lesions found no demographic patient differences but found that tumors were larger, with more microvascular invasion, in noncirrhotic HCC patients and that noncirrhotic HCC patients had more advanced tumor-node-metastasis (TNM) stage disease compared to cirrhotic patients [24]. In addition, it was noted that there were differences in postoperative morbidity (8.3–55.5%) or mortality (0–6.5%) between both groups. There is an obvious degree of selection bias in the cirrhotic population that undergoes resection as the primary treatment of HCC, but the most important difference that is seen between the two groups is in the disease-free survival (DFS). The largest multicenter report comes from the Liver Cancer Study Group from Japan and their cohort of 6,785 patients treated with resection for HCC [25]. Their cohorts’ 1-, 3-, 5-, and 10-year survival rates were noted to be 85, 64, 45 and 21%, respectively. The morbidity and mortality success rate in liver resection (LR) depends on optimizing patient selection and extent of resection to ensure adequate margin and adequate functional liver reserve (FLR) volume after resection. Several studies have demonstrated that adequate FLR be >20% in noncirrhotic livers and >40% in cirrhotics [26–28]. In addition, portal vein embolization is an important tool in the hypertrophy of the remnant liver to ensure adequate volume. A large multicenter study from France, USA, and China reviewing only major (more than segments) LRs for HCC demonstrated 3-, 5-, and 10-year overall survival (OS) of 54, 40, and 27% [29]. Factors predictive of poor long-term survival outcomes included AFP level >1,000 ng/mL, tumor size >5 cm, presence of major vascular invasion, presence of extrahepatic metastases, positive surgical margins, and earlier time period in which the major hepatectomy was performed [29].
Recurrence rates have been demonstrated to be the significant downside to surgical resection as there is an increased risk of de novo or recurrent HCC, in comparison to those patients who undergo liver replacement therapy with liver transplant(ation) (LT). Several scoring systems have been developed to predict the recurrence and OS following LR for HCC. These nomograms include the Singapore Liver Cancer Recurrence (SLICER) Score, the Surgery-Specific Cancer of the Liver Italian Program (SSCLIP) scoring system and the Memorial Sloan Kettering Cancer Center scoring system [30–32]. The scores were constructed to predict the 3- and 5-year DFS and all three identified preoperative AFP, vascular invasion and tumor size and independent predictors of successful long-term disease-free outcome. In these cohorts and other single and multi-institutional reviews, the recurrence rate after surgical resection has ranged widely [24, 33–35]. One of the largest series, collected in a prospective fashion, comes from Poon et al. and demonstrated 1-, 3-, 5- and 10-year DFS rates were 74, 50, 36, and 22% [33]. Predictors of poor recurrence rates were cirrhosis and number of lesions.
Local regional therapy is an interesting and selective effective modality for treatment of HCC. The experience with this modality comes from the patient in which LT or LR is contraindicated, in which case it has demonstrated prolonged OS. Several indications exist for the use of local regional therapy including as a primary treatment of HCC in those with early disease that are not candidates for LR or LT, a downstaging too for those with tumor size too large for successful transplant, and as a bridge therapy for those that may have a prolonged wait for cadaveric or live donor LT. Commonly used tumor ablative modalities include radiofrequency ablation (RFA), microwave ablation (MWA) or cryoablation. RFA is currently the more commonly used modality for ablative local regional therapy for primary HCC treatment, downstaging, and bridge therapy and works by tissue destruction with frictional heat generation from application of alternating current. The limitations of this modality, as it does require sustained heat generation to ensure tumor tissue necrosis with a margin, includes the “heat sink” effect that does occur from high-flow vasculature found within the liver providing for decreased temperature and therefore ineffect...