
eBook - ePub
Radiology of the Chest and Related Conditions
F W Wright
This is a test
Partager le livre
- 912 pages
- English
- ePUB (adapté aux mobiles)
- Disponible sur iOS et Android
eBook - ePub
Radiology of the Chest and Related Conditions
F W Wright
Détails du livre
Aperçu du livre
Table des matières
Citations
À propos de ce livre
The book presents a comprehensive overview of the various disease processes affecting the chest and related abnormalities. It discusses biopsy and bronchography, as well as a variety of imaging techniques including radiography, fluoroscopy, tomography, and ultrasound.
Foire aux questions
Comment puis-je résilier mon abonnement ?
Il vous suffit de vous rendre dans la section compte dans paramètres et de cliquer sur « Résilier l’abonnement ». C’est aussi simple que cela ! Une fois que vous aurez résilié votre abonnement, il restera actif pour le reste de la période pour laquelle vous avez payé. Découvrez-en plus ici.
Puis-je / comment puis-je télécharger des livres ?
Pour le moment, tous nos livres en format ePub adaptés aux mobiles peuvent être téléchargés via l’application. La plupart de nos PDF sont également disponibles en téléchargement et les autres seront téléchargeables très prochainement. Découvrez-en plus ici.
Quelle est la différence entre les formules tarifaires ?
Les deux abonnements vous donnent un accès complet à la bibliothèque et à toutes les fonctionnalités de Perlego. Les seules différences sont les tarifs ainsi que la période d’abonnement : avec l’abonnement annuel, vous économiserez environ 30 % par rapport à 12 mois d’abonnement mensuel.
Qu’est-ce que Perlego ?
Nous sommes un service d’abonnement à des ouvrages universitaires en ligne, où vous pouvez accéder à toute une bibliothèque pour un prix inférieur à celui d’un seul livre par mois. Avec plus d’un million de livres sur plus de 1 000 sujets, nous avons ce qu’il vous faut ! Découvrez-en plus ici.
Prenez-vous en charge la synthèse vocale ?
Recherchez le symbole Écouter sur votre prochain livre pour voir si vous pouvez l’écouter. L’outil Écouter lit le texte à haute voix pour vous, en surlignant le passage qui est en cours de lecture. Vous pouvez le mettre sur pause, l’accélérer ou le ralentir. Découvrez-en plus ici.
Est-ce que Radiology of the Chest and Related Conditions est un PDF/ePUB en ligne ?
Oui, vous pouvez accéder à Radiology of the Chest and Related Conditions par F W Wright en format PDF et/ou ePUB ainsi qu’à d’autres livres populaires dans Law et Forensic Science. Nous disposons de plus d’un million d’ouvrages à découvrir dans notre catalogue.
Informations
Chapter 1: Reading of Chest Radiographs Some basic Anatomy and Physiology; including Pleural Fissures, Mediastinal Lines, The Bronchi and Para-Tracheal Lines, Hilar Anatomy, the Pulmonary Lobules, Acini and Lung Cortex, Distribution of Lung Disease in Relation to Anatomy and Physiology, Basic CT and Pathological Anatomy.
DOI: 10.4324/9780429272967-1
Reading of chest radiographs.
In reading chest radiographs it is important to understand their limitations, basic anatomy and some physiology, and to have a systematic system of scrutiny. In this chapter the author goes into most of the points in some detail, as they have a profound influence on what can be seen. High KV (or similar digital) views are considered as essential by the author as the standard for most purposes, as many low KV examinations can fail to display 30% or more of the lungs, particularly the retrocardiac, and retro-diaphragmatic areas and areas hidden by the ribs.
Value of high KV technique - It is essential to have a good technique for chest radiography, as abnormalities which should be noted may otherwise be missed. In many centres chest radiographs are still taken even now with low or inadequate KV (e.g. 50 to 70), and with a 6 ft (approx. 2 metre) focus-film distance (f.f.d.). Such techniques may easily miss or inadequately demonstrate lesions in the lungs, fail to show the larger air passages and may completely miss gross mediastinal abnormalities, such as enlarged nodes, etc. Quite often the descending aorta and the various mediastinal lines are invisible within the 'white area' covered by the heart, or the domes of the diaphragm. The subcarinal area is not displayed, and masses or nodal enlargements here may be entirely missed - this probably accounts for the usual text-book statement that nodal enlargement in sarcoidosis is typically hilar, whereas the largest nodes are often in the subcarinal and azygos regions (see also p. 19.67).
Mediastinal visibility is an essential part of chest radiography, since it is only by noting the presence, displacement or absence of the normal lines, that many abnormalities will be detected. Loss of a mediastinal line or organ outline will usually indicate adjacent disease (see 'loss of silhouette sign' - p. 2.25). Air may often be seen in the oesophagus, and may be a good indicator of normality, dilatation or displacement. Two references emphasise these points:
Evans et al. (1968): Only about 25% of the lungs are unobscured on most conventional chest radiographs. Chotas and Ravin (1995): 26.4 % of lung volumes and 43 % of lung areas are obscured by the heart, mediastinum and diaphragm on many frontal chest radiographs.
Viewers used to studying fairly contrasty low KV radiographs may have some initial difficulty in interpretation of high KV or digital radiographs, but will usually soon prefer the latter (and especially digital high KV radiographs) that contain so much more information.
Because calcification may be less readily seen, a low KV radiograph may be taken as well in a few cases (Illus. HIGH & LOW KV). However for the initial detection of disease or anatomical abnormality, the high KV has so many advantages that the author is greatly surprised that it is not universally used in the UK, despite the slightly increased initial cost of such an installation. It seems quite wrong to regard as the standard chest radiograph, one which displays only about two-thirds of the lungs, and almost totally neglects the mediastinum and the larger air passages.
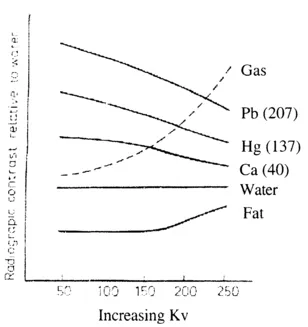
Fig. 1.1 Graph showing relationship between radiographic contrast and increasing KV for the various contrast agents and the body tissues. Numbers in brackets refer to atomic weights.
The high KV and digital techniques are further considered in Chapter 20.
| 1. Soft tissue abnormality - breasts (absence, gynaecomastia, etc.). |
| 2. Symmetry of two sides of the chest (a) lung disease. |
| (b) skeletal. |
| 3. Real or apparent increased translucency. |
| 4. Symmetry in number of blood vessels in either lung: |
| - a 50 % loss in one (or both) = loss of expansion of a major lobe, |
| - note loss of upper or lower lobe vessels (note deviation from normal pattern). |
| 5. Alteration in size of vessels |
| (a) bilateral - congestion |
| plethora (e.g. with intra-cardiac shunt) |
| oligaemia |
| (b) unilateral - Swyer James/Macleod syndrome |
| Oeser sign (spasm from hypoxia due to endobronchial obstruction). |
| (c) proximal dilatation with peripheral pruning - |
| pulmonary hypertension |
| pulmonary embolism. |
| 6. Position, patency or distortion of the trachea, carina and larger bronchi. |
| 7. Diminished volume of a lung or lobe, altered position of fissures, bronchi or pulmonary vessels. |
| 8. Obstructive emphysema (especially on expiration views). |
| 9. Intra-pulmonary consolidation, masses, nodules or other shadows, e.g. septal line engorgement, fibrosis, etc. |
| 10. Loss of part of the cardiac, aortic, SVC or diaphragmatic outline - ‘loss of outline’ or ‘loss of silhouette sign’ - see p.2.25. |
| 11. Pleural abnormality - fluid, air, thickening, mass, etc. |
| 12a. Diaphragmatic elevation caused by: - phrenic nerve palsy, eventration, secondary to lung collapse or hepatic enlargement, or mimicked by fluid or trans-diaphragmatic hernia. |
| 12b. Diaphragmatic depression caused by lung distension. |
| Note that the right side is more commonly higher than the left (see also p. 15.6). |
| 13. Presence of mediastinal and/or hilar masses - nodes, other tumours or cysts, dilated aorta, oesophagus, hiatal hernia, etc. - always study the mediastinal lines. |
| 14. Bone lesions - ribs, spine, sternum, scapulae, etc. |
| 15. Other abnormalities of the chest wall. |
| 16. Position or absence of fundal gas bubble, size of liver, site of gas in the transverse colon, etc. |
Comment: It seems a great pity that many clinicians and radiologists as well, do not really look for the signs of incomplete chest expansion (reduced volume and vessel changes), when a visual inspection of chest movement and its expansion is one of the first observations that is made in every clinical examination of the chest. This lack of appreciation of the findings in partial collapse, together with low radiographs, and the poor demonstration of the mediastinum, has been a major problem in chest radiography. CT (particularly HRCT) has greatly helped in the investigation of the mediastinum and with diffuse lung disease.
On Lateral Views (details on ps. 1.26 to 1.32).
- Similar points as on frontal views i.e. soft tissue abnormalities, symmetry, altered position of fissures, pleural fluid, visible lung (or lobe) outline indicating a pneumothorax, presence of lung, hilar or mediastinal masses, consolidation, signs of congestion, loss of silhouette - heart, diaphragm etc., elevated or 'humped' hemidiaphragm, abnormalities of visceral gas shadows, bony abnormalities, etc.
- Particular attention to:
- (i) Tracheal gas column, and stripes, carina, ring shadows of main bronchi.
- (ii) Vascular patterns in the two lungs, especially the pulmonary arteries, which have different patterns on each side (Figs. 1.33 - 1.35 and Chapter 7).
- (iii) The normally transradiant upper anterior mediastinum above the heart.
- (iv) The normally transradiant retrocardiac area.
- (v) The subcarinal area.
- (vi) Differences between the two lungs - volume, partial collapse, or over-expansion, absence of normal vascular shadows, etc.
Pleural fissures.
Oblique (or major) and horizontal (minor or lesser) fissures
The normal position of these is well known. The oblique fissures normally run from about the level of the D6 vertebral body posteriorly to the anterior costophrenic angles at about the level of the ninth costo-chondral-junction, with the left slightly more vertical and posterior in its lower part (Fig. 1.4 ). This difference in orientation is probably related to the presence of the heart on the left.
The oblique fissures do not run completely in the same plane and are somewhat obliquely orientated and undulating. Below the lower lobe bronchial levels, the central (and lateral, on the left) parts of each oblique fiss...