- English
- ePUB (mobile friendly)
- Available on iOS & Android
eBook - ePub
Respiratory Medicine
About this book
Providing a detailed overview of respiratory medicine in one short volume, Respiratory Medicine Lecture Notes covers everything from the basics of anatomy and physiology through to information on a full range of respiratory diseases.
Whether approaching the topic for the first time, starting a rotation, or looking for a quick-reference summary, medical students, specialist nurses, technicians and doctors in training will find this book an invaluable source of theoretical and clinical information.
Frequently asked questions
Yes, you can cancel anytime from the Subscription tab in your account settings on the Perlego website. Your subscription will stay active until the end of your current billing period. Learn how to cancel your subscription.
No, books cannot be downloaded as external files, such as PDFs, for use outside of Perlego. However, you can download books within the Perlego app for offline reading on mobile or tablet. Learn more here.
Perlego offers two plans: Essential and Complete
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
We are an online textbook subscription service, where you can get access to an entire online library for less than the price of a single book per month. With over 1 million books across 1000+ topics, we’ve got you covered! Learn more here.
Look out for the read-aloud symbol on your next book to see if you can listen to it. The read-aloud tool reads text aloud for you, highlighting the text as it is being read. You can pause it, speed it up and slow it down. Learn more here.
Yes! You can use the Perlego app on both iOS or Android devices to read anytime, anywhere — even offline. Perfect for commutes or when you’re on the go.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Yes, you can access Respiratory Medicine by Stephen J. Bourke,Graham P. Burns in PDF and/or ePUB format, as well as other popular books in Medicine & Pulmonary & Thoracic Medicine. We have over one million books available in our catalogue for you to explore.
Information
Part 1
Structure and Function
1
Anatomy and physiology of the lungs
The anatomy and physiology of the respiratory system are designed in such a way as to bring air from the atmosphere and blood from the circulation into close proximity across the alveolar capillary membrane in order to facilitate the exchange of oxygen and carbon dioxide.
Clinical anatomy
Bronchial tree and alveoli
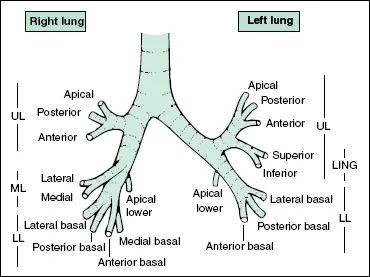
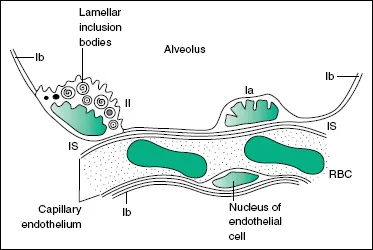
The trachea has cartilaginous horseshoe-shaped ‘rings’ supporting its anterior and lateral walls. The posterior wall is flaccid and bulges forward during coughing. The trachea divides into the right and left main bronchi at the level of the sternal angle (angle of Louis). The left main bronchus is longer than the right and leaves the trachea at a more abrupt angle. The right main bronchus is more directly in line with the trachea so that inhaled material tends to enter the right lung more readily than the left. The main bronchi divide into lobar bronchi (upper, middle and lower on the right; upper and lower on the left) and then segmental bronchi as shown in Fig. 1.1. The position of the lungs in relation to external landmarks is shown in Fig. 1.2. Bronchi are airways with cartilage in their walls, and there are about 10 divisions of bronchi beyond the tracheal bifurcation. Smaller airways without cartilage in their walls are referred to as bronchioles. Respiratory bronchioles are peripheral bronchioles with alveoli in their walls. Bronchioles immediately proximal to alveoli are known as terminal bronchioles. In the bronchi, smooth muscle is arranged in a spiral fashion internal to the cartilaginous plates. The muscle coat becomes more complete distally as the cartilaginous plates become more fragmentary. The epithelial lining is ciliated and includes goblet cells. The cilia beat with a whip-like action, and waves of contraction pass in an organised fashion from cell to cell so that material trapped in the sticky mucus layer above the cilia is moved upwards and out of the lung. This mucociliary escalator is an important part of the lung’s defences. Larger bronchi also have acinar mucus-secreting glands in the submucosa that are hypertrophied in chronic bronchitis. Alveoli are about 0.1–0.2 mm in diameter and are lined by a thin layer of cells of which there are two types: type I pneumocytes have flattened processes that extend to cover most of the internal surface of the alveoli; type II pneumocytes are less numerous and contain lamellated structures that are concerned with the production of surfactant (Fig. 1.3). There is a potential space between the alveolar cells and the capillary basement membrane that is only apparent in disease states when it may contain fluid, fibrous tissue or a cellular infiltrate.
Figure 1.1 Diagram of bronchopulmonary segments. LING, lingula; LL, lower lobe; ML, middle lobe; UL, upper lobe.
Lung perfusion
The lungs receive a blood supply from both the pulmonary and systemic circulations. The pulmonary artery arises from the right ventricle and divides into left and right pulmonary arteries, which further divide into branches accompanying the bronchial tree. The pulmonary capillary network in the alveolar walls is very dense and provides a very large surface area for gas exchange. The pulmonary venules drain laterally to the periphery of lung lobules and then pass centrally in the interlobular and intersegmental septa, ultimately joining to form the four main pulmonary veins that empty into the left atrium. Several small bronchial arteries usually arise from the descending aorta and travel in the outer layers of the bronchi and bronchioles supplying the tissues of the airways down to the level of the respiratory bronchiole. Most of the blood drains into radicles of the pulmonary vein contributing a small amount of de-saturated blood that accounts for part of the ‘physiological shunt’ (blood passing through the lungs without being oxygenated) observed in normal individuals. The bronchial arteries may undergo hypertrophy when there is chronic pulmonary inflammation, and major haemoptysis in diseases such as bronchiectasis or aspergilloma usually arises from the bronchial rather than the pulmonary arteries and may be treated by therapeutic bronchial artery embolisation. The pulmonary circulation normally offers a much lower resistance and operates at a lower perfusion pressure than the systemic circulation. The pulmonary capillaries may be compressed as they pass through the alveolar walls if alveolar pressure rises above capillary pressure.
Figure 1.2 Surface anatomy. (a) Anterior view of the lungs. (b) Lateral view of the right side of chest at resting endexpiratory position. LLL, left lower lobe; LUL, left upper lobe; RLL, right lower lobe; RML, right middle lobe; RUL, right upper lobe.
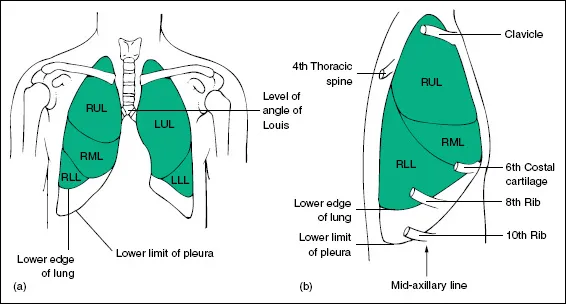
Figure 1.3 Structure of the alveolar wall as revealed by electron microscopy. Ia, type I pneumocyte; Ib, flattened extension of type I pneumocyte covering most of the internal surface of the alveolus; II, type II pneumocyte with lamellar inclusion bodies that are probably the site of surfactant formation; IS, interstitial space; RBC, red blood corpuscle. Pneumocytes and endothelial cells rest upon thin continuous basement membranes that are not shown.
Physiology
The core business of the lungs is to bring oxygen into the body and to take carbon dioxide out.
This is brought about by a process best considered in two steps:
1 moving air in and out of the lungs (between the outside world and the alveoli);
2 gas exchange: the exchange of oxygen and carbon dioxide between the airspace of the alveoli and the blood.
This process continues throughout life largely unconsciously, coordinated by a centre in the brain stem. The factors that regulate the process, ‘the control of breathing’ will also be considered here.
Moving air in and out of the lungs
To understand this process we need to consider the muscles that ‘drive the pump’ and the resistive forces they have to overcome. These forces include the inherent elastic property of the lungs and the resistance to airflow through the bronchi (airway resistance).
The muscles that drive the pump
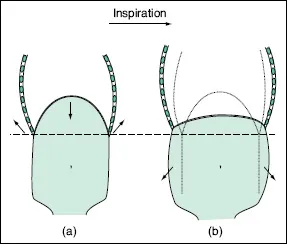
Inspiration requires muscular workInspiration requires muscular work. The diaphragm is the principal muscle of inspiration. At the end of the previous expiration the diaphragm sits in a soft, domed position high in the thorax (Fig. 1.4). To inspire, the strong muscular sheet contracts, it stiffens and tends to push the abdominal contents down. There is variable resistance to this downward pressure by the abdomen; which means that to accommodate the new shape of the diaphragm the lower ribs (to which it is attached) also move upwards and outwards. The degree of resistance the abdomen presents can be voluntarily increased by contracting the abdominal muscles, inspiration then leads to a visible expansion of the thorax. The resistance may also be increased by abdominal obesity. In such circumstances there is an involuntary limitation to the downward excursion of the diaphragm and, as the potential for upward movement of the ribs is limited, the capacity for full inspiration is diminished. This inability to fully inflate the lungs is an example of a restrictive ventilatory defect (see Chapter 3).
Figure 1.4 Effect of diaphragmatic contraction. Diagram of the ribcage, abdominal cavity and diaphragm showing the position at the end of resting expiration (a). As the diaphragm contracts it pushes the abdominal contents down (the abdominal wall moves outwards) and reduces pressure with the thorax which ‘sucks’ air in through the mouth (inspiration). As the diaphragm shortens and descends it also stiffens. The diaphragm meets a variable degree of resistance to downward discursion that forces the lower ribs to move up and outward to accommodate its new position (b).
Other muscles are also involved in inspiration. The scalene muscles elevate the upper ribs and sternum. These are active even in quiet breathing although they were once considered, along with the sternocleidomastoids, as ‘accessory muscles of respiration’, only brought into play during the exaggerated ventilatory effort of acute respiratory distress.
The intercostal muscles bind the ribs to ensure the integrity of the chest wall. They therefore transfer the effects of actions on the upper or lower ribs to the whole rib cage. They also brace the chest wall, resisting the bulging or indrawing effect of changes in pleural pressure during breathing. This bracing effect can be overcome to some extent by the exaggerated pressure changes seen during periods of more extreme respiratory effort, and in slim individuals intercostal recession may be observed as a sign of respiratory distress.
Whereas inspiration is the result of active muscular effort, quiet expiration is a more passive process. The inspiratory muscles steadily release their contraction and the elastic recoil of the lungs brings the tidal breathing cycle back to its start point. Forced expiration however, either volitional or as in coughing for example, requires muscular effort. T...
Table of contents
- Cover
- Title
- Copyright
- Preface
- Part 1: Structure and Function
- Part 2: History Taking, Examination and Investigations
- Part 3: Respiratory Diseases
- Part 4: Self-assessment
- Index