- 328 pages
- English
- ePUB (mobile friendly)
- Available on iOS & Android
About this book
This excellent book is long overdue. It will be of benefit to anyone with an interest in general practitioner education, and anyone considering applying for the post of course organiser should read the opening chapters to prepare them for interview. This is a thoughtful book, written in a clear and witty style and it deserves a wide readership. It provides an educational framework on which general practitioner teaching can be based.' British Journal of General Practice This book is excellent because it deals not only with the nuts and bolts' of being a course organizer, but also addresses the difficulties, frustrations and emotions involved in a witty and entertaining manner. Anyone with an interest in postgraduate medical education, at any level, would benefit from reading this book.' Update Paddy McEvoy's book has rapidly and deservedly established itself as invaluable to anyone responsible for any form of postgraduate medical education.' Education for General Practice 'As well as updating and revising the book throughout. Paddy McEvoy has managed to include sections about the wider context of training without making the book overly long or losing any of the delightful flavour of the first edition. I have no doubt that you will find it both useful and enjoyable.''
Frequently asked questions
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Information
Chapter 1
The policy context for substance misuse services in primary care
What’s happening to primary care?
- It exists in the real world.
- It is local.
- It is accessible and realistic.
- It is long term.
- It takes a ‘full-length feature film look’ at people’s lives in the context of their health.
- ‘Snapshots’, although useful, belong more in rescue medicine than planned holistic management of chronic health problems which is the strength of primary care.
- It needs to be patient centred but often it isn’t.
Stop here
- In your practice, are you confident you apply these principles to your patients with substance misuse problems?
- Could you pick up one of your existing cases and quickly establish:
- – the initial treatment goals
- – the motivational factors for behavioural change
- – the actions to be taken if review reveals unmet need or variance from direction of progress?
Contracts in context
Box 1.1 Changes in substance misuse work after the new GMS contract
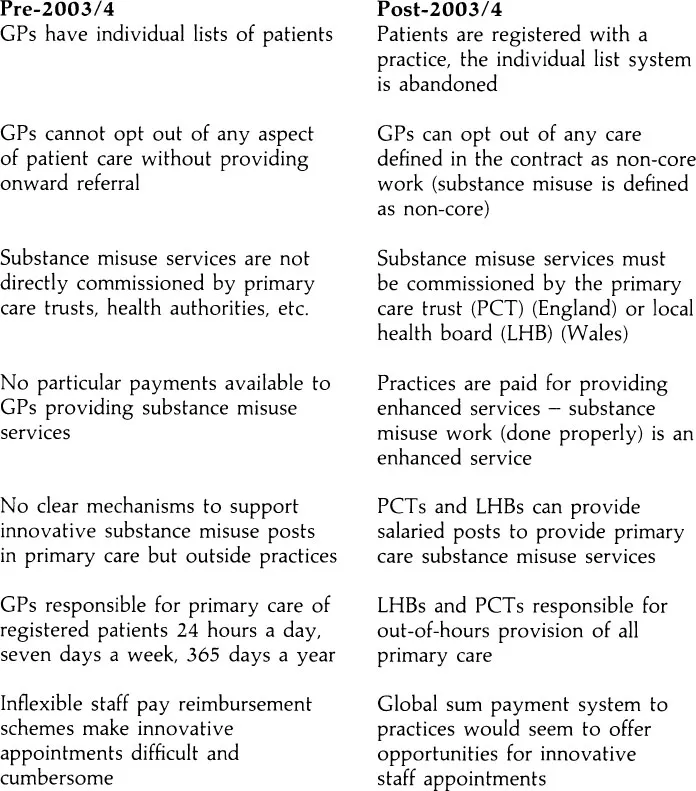
Box 1.2 Example of change in patient handling
Stop here
- Did you attend all those practice development meetings last year?
- Did you plan for this enormous shift in attitude?
The access agenda
- What is your practice doing about access?
- Are you involved in the processes of change? (If not why not?)
- Do you have untapped potential?
- Is your team aware of it? Do you need to speak with the practice manager today?
Innovation and service development
Box 1.3
Table of contents
- Cover
- Title Page
- Copyright Page
- Contents
- Foreword
- Preface
- About the editor
- List of contributors
- List of abbreviations
- Chapter 1 The policy context for substance misuse services in primary care
- Chapter 2 Practical guide for the addiction nurse in shared care
- Chapter 3 Users and practitioners: an equal partnership
- Chapter 4 The role of the practice nurse in substance misuse treatments
- Chapter 5 Primary care nursing and alcohol: a new way forward?
- Chapter 6 The role of the midwife working with a pregnant drug user
- Chapter 7 The role of the health visitor in relation to child protection and substance misuse
- Chapter 8 Treatment and its effectiveness in relapse prevention associated with crack cocaine
- Chapter 9 The role of the practice counsellor in substance misuse treatments
- Chapter 10 Special issues for effective treatment of homeless drug users
- Chapter 11 The complex world of dual diagnosis, nursing and primary care
- Chapter 12 Future directions and partnerships: the way forward for nursing
- Appendix 1 Sample methadone prescribing protocol
- Appendix 2 Sample Subutex prescribing protocol
- Appendix 3 Luther Street policy for the management of contacts with the addictions team
- Appendix 4 DANOS competencies for addiction nurses
- Index