- 338 pages
- English
- ePUB (mobile friendly)
- Available on iOS & Android
Nutritional Signaling Pathway Activities in Obesity and Diabetes
About this book
Nutrients can act as signalling molecules to initiate or mediate signalling transduction that regulates cell function and homeostasis. As such, altered nutrient status has been linked to dysregulated transcripts and protein expression, which affects mitochondrial function, autophagy, inflammation, metabolism and even gut microbiota. This book disseminates the cutting-edge knowledge pertaining to nutritional signalling activities in metabolism and metabolic derangements (e.g., obesity and diabetes), which covers the regulatory mechanisms and dietary interventions for disease prevention.
This book represents current nutritional and metabolic research. From the basic (molecular science) perspective, it covers metabolomics, proteomics, nutrigenomics, nuclear receptors and transcription factors, inflammatory pathways, autophagy, mitochondrial health and gut microbiota. From the clinical (translational science) perspective, this book covers clinical trials, precision nutrition, maternal nutrition and transgenerational health, and allometric scaling of dietary bioactives in translational metabolic research. It brings to the reader in-depth understanding of the nutritional aspect, cellular and molecular biology, as well as pathophysiology of obesity and diabetes. In addition, each chapter in this book includes a component of future direction or intervention perspective, making the new knowledge transformative and translational. Aimed at researchers and professionals interested in nutrition, dietetics and metabolic disorders, this book will also appeal to health science researchers.
Frequently asked questions
- Essential is ideal for learners and professionals who enjoy exploring a wide range of subjects. Access the Essential Library with 800,000+ trusted titles and best-sellers across business, personal growth, and the humanities. Includes unlimited reading time and Standard Read Aloud voice.
- Complete: Perfect for advanced learners and researchers needing full, unrestricted access. Unlock 1.4M+ books across hundreds of subjects, including academic and specialized titles. The Complete Plan also includes advanced features like Premium Read Aloud and Research Assistant.
Please note we cannot support devices running on iOS 13 and Android 7 or earlier. Learn more about using the app.
Information
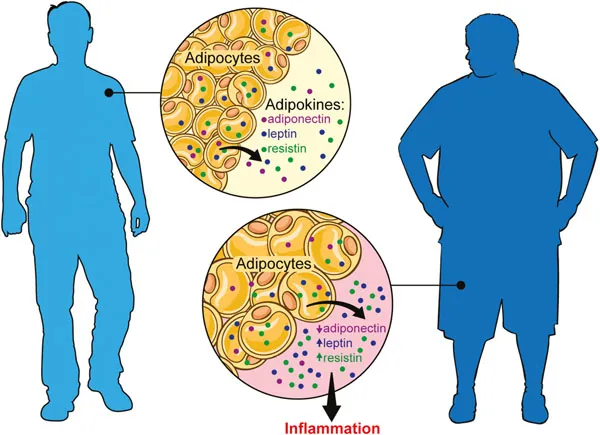
Table of contents
- Cover
- Half Title
- Series Information
- Title Page
- Copyright Page
- Preface
- Contents
- Chapter 1 Diabetes and Obesity: An Overview of Nutritional Effects
- Chapter 2 Maternal Nutrition and the Risk of Obesity and Diabetes in the Offspring
- Chapter 3 Lessons Learned from Recent Clinical Trials Targeting Diets to Treat and Prevent Obesity and Diabetes
- Chapter 4 Nutritional Regulation of Inflammation in Obesity and Diabetes
- Chapter 5 The Interaction of Nutrition with Nuclear Receptors in Obesity and Diabetes
- Chapter 6 Nutritional Regulation of Mitochondrial Health and Its Implication in Treating Obesity and Diabetes: Lessons Learned From the Resveratrol–Sirt1 Axis
- Chapter 7 The Role of Intestinal Microbiota and Microbial Metabolites in the Development of Host Metabolic Syndrome
- Chapter 8 Metabolomics in Nutritional Metabolism, Obesity, and Diabetes
- Chapter 9 Proteomics in Nutrition, Obesity and Diabetes Research
- Chapter 10 Personalized Nutrition to Treat and Prevent Obesity and Diabetes
- Chapter 11 Allometric Scaling of Dietary Bioactives in Metabolic Research: The Present and Future
- Subject Index