Biological Sciences
History of Antibiotics
The history of antibiotics dates back to the discovery of penicillin by Alexander Fleming in 1928. This breakthrough revolutionized medicine by providing a powerful tool to combat bacterial infections. Over the years, numerous other antibiotics have been developed, contributing to significant advancements in healthcare and the treatment of infectious diseases.
Written by Perlego with AI-assistance
Related key terms
1 of 5
8 Key excerpts on "History of Antibiotics"
- eBook - PDF
- H. van der Goot(Author)
- 2002(Publication Date)
- Elsevier Science(Publisher)
H. van der Goot (Editor) Trends in Drug Research III © 2002 Elsevier Science B.V. All rights reserved 193 Antibacterials as Wonder Drugs and How Their Effectiveness Is Being Compromised Dasantila Golemi,§ Laurent Maveyraud,* Jalal Haddad, Wenlin Lee, Akihiro Ishiwata,§ Kazuyuki Miyashita,§ Lionel Mourey,+ Sergei Vakulenko, Lakshmi Kotra, Jean-Pierre Samama,-!- and Shahriar Mobashery,§* •••Groupe de Cristallographie Biologique, Institut de Pharmacologic ct de Biologic Structurale du CNRS, 205 route dc Narbonnc, 31077-Toulousc ccdcx, France ^Department of Chemistry and Institute for Drug Design, Wayne State University, Detroit, MI 48202-3489 USA. Treatment of infections by bacterial pathogens became possible only in the twentieth century. Indeed, virtually all classes of antibacterials that are in clinical use presently were discovered and developed in the span of a mere 30 or so years. The advent of antibiotics, along with immunization, has had profound consequences on the quality of life. Life expectancy increased in the United States by 30 years from the beginning to the end of the twentieth century, as a direct consequence of these developments [1]. These successes created an air of complacency. There was the perception that bacterial infections were infinitely curable. This view was strengthened by the late 1960s into 1970s, in part because of the discoveries of the various classes of antibiotics, but also by the fact that medicinal chemists appeared to be able to improve these molecules of natural origins by synthetically altering them. These synthetic molecules were often more potent that their parental natural products, and at times the breadth of activities were also increased to create pharmaceuticals that were being hailed as miraculous in the clinic. The euphoria lead to complacency, such that by the late 1980s and earlier 1990 many pharmaceutical companies decided to leave the field of antibiotics. - eBook - PDF
Challenges to Tackling Antimicrobial Resistance
Economic and Policy Responses
- Michael Anderson, Michele Cecchini, Elias Mossialos, Jonathan North(Authors)
- 2020(Publication Date)
- Cambridge University Press(Publisher)
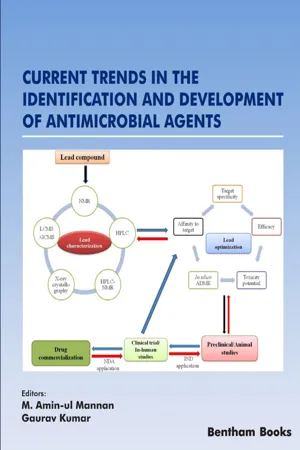
Antimicrobial resistance is a broader term, encompassing resistance to drugs to treat infections caused by other microbes as well, such as par- asites (e.g. malaria), viruses (e.g. HIV) and fungi (e.g. Candida). In this book we normally refer to antibiotics unless otherwise indicated but we retain the abbreviation AMR because it is in common use. Antimicrobial resistance is a biological mechanism whereby a microorganism evolves over time to develop the ability to become resistant to antimicrobial therapies such as antibiotics. The discovery of antibiotics has been one 2 Challenges to Tackling Antimicrobial Resistance of the most significant developments for humanity over the last 70 years – a breakthrough in the treatment of communicable diseases which has also facilitated developments in other areas of medicine such as surgery, obstetrics and oncology (Holmes et al., 2016; Teillant et al., 2015). The development of AMR is intrinsic to the use of antibiotics but its growth and spread is exacerbated by their overuse and misuse. This risk has been known for a long time. Sir Alexander Fleming, the discoverer of penicillin, noted this in an interview as early as 1945: In such cases, the thoughtless person playing with penicillin is morally responsible for the death of the man who finally succumbs to infection with the penicillin-resistant organism. I hope this evil can be averted (New York Times, 1945). The widespread dissemination of antibiotics in the succeeding decades only increases the relevance of his words today. Following the discovery of penicillin in 1928, many classes of antibiotics followed; a period many describe as the “golden era” of antibiotic discovery. Despite this initial expansion, in the last 30 years there has been a dearth of novel antibiotics discovered (Freire-Moran et al., 2011; Spellberg et al., 2004). Globally, the prevalence rate of resistant bacteria has been steadily increasing. - M. Amin-ul Mannan, Gaurav Kumar, M. Amin-ul Mannan, Gaurav Kumar(Authors)
- 2008(Publication Date)
- Bentham Science Publishers(Publisher)
Anti Bacterial Drugs: A Bright Past but a Challenging FutureNitin Pal Kalia1,Manoj Kumar2,Souhaila Al Khodor2,Sandeep Sharma3 , *1 Department of Biological Sciences (Pharmacology & Toxicology), National Institute of Pharmaceutical Education and Research (NIPER), Hyderabad, Telangana, India2 Department of Research, Sidra Medicine, Doha, Qatar3 Department of Medical Laboratory Sciences, Lovely Professional University, Phagwara, Punjab, IndiaAbstract
The discovery of penicillin opened the avenues for antibacterial drug discovery to address the global problem of deadly infectious diseases. However, despite the availability of potent antibiotics and effective vaccines, bacterial infections are still the major contributors to morbidity and mortality worldwide. The use of antibiotics is a two-edged sword; on the one hand, antibiotics have helped us combat deadly bacterial infections. On the other hand, overuse of antibiotics has led bacterial pathogens to develop drug resistance. The components of the bacterial cell-like cell wall, cell membrane, protein synthesis, and nucleic acid synthesis were targeted to develop effective drugs. Using these selective microbial targets, multiple potent antibiotic classes were developed in the last century, but emerging bacterial resistance and a decline in the number of new antibiotic approvals in recent years are pushing us back to the pre-antibiotic era. An increase in multidrug-resistant strains and the ineffectiveness of current drugs pose a challenge for researchers to develop new antibiotics with a novel mechanism to treat drug resistance. In the current chapter, we focus on the antibacterial drug used for the treatment of important human pathogens.- Carlos F. Amabile-Cuevas(Author)
- 2015(Publication Date)
- CRC Press(Publisher)
Chapter 1 Definitions and basic concepts When thinking of “antibiotics in the environment’’, perhaps a first image that comes to mind is a clandestine dumping of antibiotics from a drug factory into a river in a non-developed country; and when thinking of “antibiotic resistance in the environment’’, the natural consequence would be to think of an aquatic bacteria under the selection of the dumped antibiotic becoming resistant to the drug, and then causing an outbreak in a neighboring town. The actual scenario is far more complicated and complex: com-plicated, as there are much more elements at play; complex, as the interactions of those elements are many and multi-directional. Even from the semantic point of view, there could be confusion as to what we call “antibiotic’’, “resistance’’ or “environment’’, so it is important to begin with some working definitions. Although some definitions are not unanimously agreed upon, it is crucial to frame the content of this book within those definitions, in order to avoid misinterpretation. In addition to formal definitions, this first section will deal with some concepts that are relevant and necessary to understand the reach and limitations of our cur-rent knowledge of the topic at hand. What is the “role’’ of natural antibiotics in microbial ecology? How is the definition of resistance limiting the perspective view of its emergence and evolution? What are the advantages and disadvantages of using molecular-based or culture-based techniques for assessing resistance in the environ-ment? Many of these issues are clearly controversial, and the author’s bias will become clear; but by actually stating a position, it is hoped that the readers will be able to reach their own conclusions much more easily.- eBook - PDF
- Nina Parker, Mark Schneegurt, Anh-Hue Thi Tu, Brian M. Forster, Philip Lister(Authors)
- 2016(Publication Date)
- Openstax(Publisher)
Chapter 14 Antimicrobial Drugs Figure 14.1 First mass produced in the 1940s, penicillin was instrumental in saving millions of lives during World War II and was considered a wonder drug. [1] Today, overprescription of antibiotics (especially for childhood illnesses) has contributed to the evolution of drug-resistant pathogens. (credit left: modification of work by Chemical Heritage Foundation; credit right: modification of work by U.S. Department of Defense) Chapter Outline 14.1 History of Chemotherapy and Antimicrobial Discovery 14.2 Fundamentals of Antimicrobial Chemotherapy 14.3 Mechanisms of Antibacterial Drugs 14.4 Mechanisms of Other Antimicrobial Drugs 14.5 Drug Resistance 14.6 Testing the Effectiveness of Antimicrobials 14.7 Current Strategies for Antimicrobial Discovery Introduction In nature, some microbes produce substances that inhibit or kill other microbes that might otherwise compete for the same resources. Humans have successfully exploited these abilities, using microbes to mass-produce substances that can be used as antimicrobial drugs. Since their discovery, antimicrobial drugs have saved countless lives, and they remain an essential tool for treating and controlling infectious disease. But their widespread and often unnecessary use has had an unintended side effect: the rise of multidrug-resistant microbial strains. In this chapter, we will discuss how antimicrobial drugs work, why microbes develop resistance, and what health professionals can do to encourage responsible use of antimicrobials. 14.1 History of Chemotherapy and Antimicrobial 1. “Treatment of War Wounds: A Historical Review.” Clinical Orthopaedics and Related Research 467 no. 8 (2009):2168–2191. Chapter 14 | Antimicrobial Drugs 603 - eBook - PDF
Antimicrobial Resistance
A Global Threat
- Yashwant Kumar(Author)
- 2019(Publication Date)
- IntechOpen(Publisher)
Chapter 1 Introductory Chapter: Stepping into the Post-Antibiotic Era—Challenges and Solutions Neelam Taneja, Shveta Sethi, Ajay Kumar Tahlan and Yashwant Kumar Additional information is available at the end of the chapter http://dx.doi.org/10.5772/intechopen.84486 1. Antibiotics and antibiotic resistance in the pre-antibiotic era Antibiotics are known to exist in the history of mankind since ancient times. They can be traced back to as early as 350–550 CE, when scientists found traces of tetracycline inhuman skeletal remains of ancient Sudanese Nuba [1]. This has led to the speculation that the diet of this population contained tetracycline. Even the red soils of Jordon which have been used since time immemorial to treat wounds have been shown to contain Actinomycete bacteria which produced actinomycin [2]. Antimicrobial activity is also present in many of the herbs used in traditional Indian Ayurvedic and Chinese medicines. Antibiotics have saved countless lives, and at one point of time, we imagined that infectious diseases were conquered. Most of the advances of modern medicine including state of art sur-geries and management of neutropenic, transplant and cancer patients are based on the use of effective broad-spectrum antibiotics. Thanks to the way we have handled these precious resources for treatment of variety of infectious diseases. However, we found to our dismay subsequently that we are stepping into the post-antibiotic era. Antibiotic resistance genes have been present in nature long before the modern antibiotic era began. Some of the serine and metallo-beta-lactamases originated more than 2 million years ago [3]. It seems prudent to assume that the ancient bacteria had defence mechanisms (such as antibiotic altering enzymes or efflux pumps) to protect themselves from high antibiotic con -centrations. - Arti Gupta, RAM PRASAD, Arti Gupta, RAM PRASAD(Authors)
- 2023(Publication Date)
- CRC Press(Publisher)
However, during the early 1900s, most of the global population suffered from common ailments, namely cold and flu, owing to the paucity of antimicrobial agents. The substances that inhibit the growth and development of microorganisms such as bacteria, viruses, protozoa and fungi are called antimicrobials (Burnett-Boothroyd and McCarthy 2011). The term antibiotic, on the other hand, originates from antibiosis which means ‘against life’. Earlier, the use of this term was confined to the natural chemical ingredients produced by microbes that were either lethal (bactericidal) or inhibitory (bacteriostatic) to other related microorganisms (such as algae, bacteria and fungi) but now they also include chemically-synthesized compounds (Aminov and Mackie, 2007 ; Amnirov, 2009). Till now, ~250 types of antibiotics have been noted for use in humans and animals where they have been shown to affect the biosynthesis of components of cell wall, protein synthesis machinery, folic acid synthesis, metabolism and genetic element of the organisms (Figure 4.1 ; Kummerer, 2003 ; Singh et al., 2021). The prime source for antimicrobials/antibiotics includes algae, bacteria, fungi and plants (Hayashi et al., 2014; Inamuddin et al. 2021). With advances in therapeutics, the multitude of antibiotics usage and lack of surveillance gathered crucial setbacks, of which acquired resistance is the prominent one. Bacterial resistance can be categorized into multidrug-resistant (MDR), pan drug-resistant (PDR) and extreme drug-resistant (XDR) (Magiorakos et al., 2012). MDR bacteria have become an alarming concern owing to their steadily growing resistance to last drug resorts such as vancomycin and colistin- eBook - PDF
Food Microbiology
In Human Health and Disease
- Nancy Khardori(Author)
- 2016(Publication Date)
- CRC Press(Publisher)
CHAPTER 8 Antibiotic Use in Animal Feed and its Impact on Antibiotic Resistance in Human Pathogens Daniel P. Ballard, Emily A. Peterson, Joseph L. Nadler and Nancy M. Khardori * Introduction Along with the development of vaccines, antimicrobial agents are widely regarded as one of the most important advances in modern medicine. Prior to the discovery of antibiotics, common infections often resulted in death. Antibiotics have made possible the treatment and prevention of diseases which were previously responsible for incredible morbidity and mortality both in children and adults. After Alexander Fleming discovered penicillin in 1928, the drug was celebrated as a miracle cure. Today, antimicrobial drugs have become easily available, relatively non-toxic and have therefore fallen prey to overuse and abuse. The collateral damage associated with their appropriate use, overuse and abuse are all associated with the development of resistance to these lifesaving agents. Division of Infectious Diseases, Department of Internal Medicine Eastern Virginia, Medical School, Norfolk, Virginia. * Corresponding author: [email protected] 138 Soon after penicillin use became widespread in the 1940s, the problem of antibiotic resistance became apparent. In his Nobel lecture, Fleming proved his incredible foresight in the light of today’s battle with antimicrobial resistance: “There may be a danger, though, in underdosage. It is not difficult to make microbes resistant to penicillin in the laboratory by exposing them to concentrations not sufficient to kill them, and the same thing has occasionally happened in the body. The time may come when penicillin can be bought by anyone in the shops. Then there is the danger that the ignorant man may easily underdose himself and by exposing his microbes to non-lethal quantities of the drug make them resistant” (Fleming 1945).
Index pages curate the most relevant extracts from our library of academic textbooks. They’ve been created using an in-house natural language model (NLM), each adding context and meaning to key research topics.