![]()
Chapter 1
Functional Renal Physiology and Urine Production
Urinalysis can provide insight into hydration status, renal function or dysfunction, systemic disease, and toxic insults. Accurate interpretation of urinalysis results requires knowledge of renal physiology and urine formation.
Given the complexity of both, a brief overview is presented below; more detailed explanations can be found in a variety of references on which this chapter is based (Gregory 2003; Kaneko 2008; Schrier 2007; Stockham and Scott 2008; Watson 1998).
Descriptions of renal function and schematics of the kidney typically portray a single nephron, which is the functional unit of the kidney; each kidney contains hundreds of thousands of nephrons working in unison (Reece 1993). Each nephron requires:
(1) A blood supply
(2) A functional glomerulus, which filters a portion of the renal blood flow, to form an ultrafiltrate
(3) Renal tubules that function to reabsorb water, electrolytes, and other substances from the ultrafiltrate
(4) Collecting tubules and ducts, which further reabsorb or excrete water and solutes and thus determine final urine concentration.
Urine formation starts as an ultrafiltrate formed by glomerular filtration. The ultrafiltrate is then further altered by tubular reabsorption and secretion.
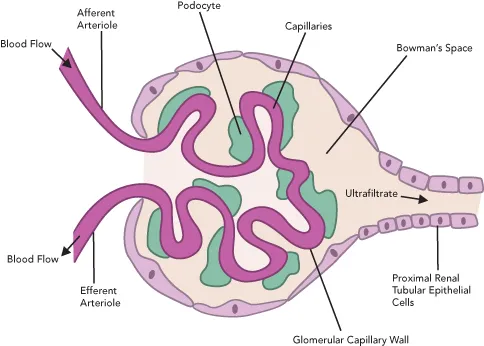
Glomerular Filtration
The glomerulus is a collection of twisted capillaries that receive blood from the afferent arteriole of the renal blood supply and exit the kidney via the efferent arteriole (Figure 1.1). The high pressure within this system results in passage of fluids and small substances out of the capillaries into a space around the glomerulus, known as Bowman’s capsule, which together form a renal corpuscle. Glomerular filtration is driven by both blood volume and pressure and is considered a primarily passive process. Ultrafiltrate is the product of glomerular filtration of blood following its passage through a glomerular filtration barrier, the glomerular capillary wall (GCW). The GCW prevents entry of red and white blood cells, platelets, and larger proteins into the ultrafiltrate. The exact composition and function of the GCW is the subject of intense research and debate currently in the human literature. Additional information is presented about glomerular filtration and the GCW in Chapter 6, “Proteinuria.”
Concentrations of urea, creatinine, amino acids, glucose, bicarbonate, and electrolytes are similar between the ultrafiltrate and plasma. Specific gravity (SG) which ranges from 1.008 to 1.012 and osmolality (300 mOsm/kg with a range of 280–310 mOsm/kg) will also be similar between the two (Watson 1998). Note the SG range of 1.008–1.012 is identical to the range described for isosthenuria. For additional information regarding interpretation of urine specific gravity (USG), see Chapter 3. Knowledge of this range is relevant for the diagnosis of renal failure as well as the interpretation of urine with an SG of less than 1.008. Chapter 3, “Routine Urinalysis: Physical Properties,” discusses USG in greater detail.
Renal blood flow ultimately determines the glomerular filtration rate (GFR) or rate of blood flow within the glomerulus. GFR can be affected by numerous factors such as a patient’s blood volume, cardiac output, and total number of functional glomeruli (Stockham and Scott 2008). GFR and direct and indirect measures of GFR can therefore be influenced by renal disease as well as nonrenal factors such as dehydration, severe blood loss, hypotension, diuretic use, fluid therapy, and hypoalbuminemia to name a few.
Ultrafiltrate exiting Bowman’s capsule enters into the proximal convoluted tubule (PCT).
Tubular Reabsorption and Secretion
Tubular reabsorption and secretion employ both passive and active mechanisms to ultimately form urine, conserve water and necessary solutes, and excrete waste products. The renal tubules are divided into the PCT, ascending and descending loops of Henle, distal convoluted tubule, and the collecting duct. Each segment serves to reabsorb and/or secrete water and various solutes (Figure 1.2). Reabsorption serves to prevent water and solutes from being excreted into the tubular fluid while secretion results in loss of either into the tubular fluid. Water and solutes remaining in the tubular fluid are excreted as urine.
Proximal Convoluted Tubule
The majority of water and solutes are reabsorbed in the PCT. Sodium is actively reabsorbed in the PCT via several mechanisms and water follows passively. In addition to sodium reabsorption, conservation of amino acids, glucose, phosphate, chloride, potassium, and bicarbonate occurs in the PCT. Fluid in the PCT displays only mild increases in SG and osmolality relative to the ultrafiltrate. Ultimately, water conservation reduces the volume of tubular fluid by 70% (Kaneko 2008; Stockham and Scott 2008; Watson 1998).
Loop of Henle
The loop of Henle includes a descending loop and ascending loop that serve to reabsorb more water and electrolytes through both passive and active mechanisms. The renal medullary interstitium, which is the tissue and fluid surrounding the tubules, and peritubular capillaries are integral parts of the conservation of water and electrolytes.
The descending loop of Henle is permeable to water but is impermeable to electrolytes. As the loop descends into the renal medulla, which is maintained at a higher osmolality due to higher concentrations of both sodium and urea, the water will exit the loop in an attempt to equilibrate with the surrounding interstitium, thus serving to conserve water. As water exits the tubular fluid, the osmolality and SG greatly increase as the tubular fluid prepares to enter the ascending loop.
The ascending loop of Henle is opposite to the descending loop and is permeable to urea and electrolytes (mostly sodium, chloride, and potassium) but impermeable to water. Tubular fluid ascends the loop of Henle and becomes increasingly more dilute as sodium and chloride are first passively and then actively reabsorbed into the medullary interstitium. Medullary interstitial hypertonicity results from the increase in sodium concentration.
Blood vessels, specifically peritubular capillaries that parallel the loop of Henle, are termed the “vasa recta.” Blood in the vasa recta flows in the opposite direction to the fluid in the loop of Henle. The loop of Henle, together with the vasa recta and interstitium, comprise a countercurrent system. The process of countercurrent multiplication is essential in maintaining a concentration gradient within the medullary interstitium as both the descending loop of Henle and collecting ducts require a hypertonic medullary interstitium for water reabsorption. Therefore, the hypertonicity of the medullary interstitium is a product of the descending loop of Henle as described above. A basic understanding of this gradient aids in interpreting extrarenal influences on urine concentration and will be discussed below (Gregory 2003; Kaneko 2008; Schrier 2007; Stockham and Scott 2008; Watson 1998).
Distal (Convoluted) Tubule
The epithelial cells of the distal tubule demonstrate minimal permeability to water. Sodium and chloride, however, can be reabsorbed from the tubular fluid in this segment primarily under the influence of aldosterone, antidiuretic hormone (ADH), and other substances.
Collecting Tubules
Although the majority of water and solute reabsorption occurs in the PCT and loop of Henle, the collecting tubules determine the final urine volume and USG. The collecting tubule is impermeable to water except in the presence of ADH, which results in reabsorption of water. ADH levels ultimately determine whether urine will be dilute or concentrated. High concentrations of urea, sodium, or chloride in the medullary interstitium facilitate ADH reabsorption of water, again reinforcing the necessity of a hypertonic renal medullary interstitium. In the absence of ADH, dilute urine is produced.
Renal function and measures of Renal Function
In the normal state, the goal of the kidneys is to conserve water, glucose, amino acids, sodium, chloride, bicarbonate, calcium, magnesium, and most proteins, and to excrete urea, creatinine, phosphate, potassium, hydrogen ions, ammonium, ketones, bilirubin, hemoglobin, and myoglobin (Stockham and Scott 2008). Additional roles of the kidneys include, but are not limited to, erythropoietin synthesis to stimulate red blood cell development, acid–base regulation, renin secretion, calcium and phosphorous homeostasis, and blood pressure regulation. Urea nitrogen (UN) and creatinine are both waste products of metabolism and are filtered and excreted by the kidneys into the urine.
Urea Production and Excretion
The liver converts ammonia, which is a product of intestinal protein catabolism, into urea. Urea, following release by the liver into the blood, is freely filtered by the glomerulus and enters the ultrafiltrate. Urea follows water into and out of the renal tubules. The amount of urea excreted in the urine varies from 40% to 70% of the ultrafiltrate and is mostly determined by flow rate within the tubules (Schrier 2007). At higher urine flow rates (i.e. increased water or fluid intake), less urea is reabsorbed and so more is excreted in the urine. Decreased urine flow rate (i.e. dehydration) results in a greater amount of urea reabsorption and so less is excreted into the urine.
Creatinine Excretion
Creatinine is produced at a constant rate from normal muscle metabolism where creatine in muscle is converted to creatinine (Gregory 2003; Kaneko 2008; Stockham and Scott 2008). Creatine concentrations are influenced by an animal’s muscle mass and underlying disease states. Similar to urea, creatinine is freely filtered by the glomerulus, meaning it passes through the glomerular filtration barrier and enters into the tubular fluid. In contrast to urea, creatinine is not reabsorbed by the renal tubules. A small amount of creatinine, however, is excreted by the proximal tubule in male dogs.
Laboratory Assessment of Renal Function
Urea and creatinine concentrations are the most commonly utilized tests to evaluate renal function. Urea concentration, typically measured in serum or plasma, is reported as UN or blood urea nitrogen (BUN). The amount of urea in whole blood, serum, or plasma is identical because urea rapidly equilibrates between compartments. Because of the variability in the amount of urea presented to the kidney and the potential for tubular reabsorption of urea, both nonrenal and renal factors influence BUN. Creatinine is a more accurate measure of GFR given its constant rate of formation and lack of tubular reabsorption (Kaneko 2008; Stockham and Scott 2008).
Azotemia
An increase in BUN and creatinine is termed azotemia. Azotemia can be prerenal, renal, or postrenal in origin although causes may be multifactorial. Prerenal azotemia results from decreased renal blood flow. Examples of prerenal azotemia include hypovolemia due to dehydration or hemorrhage, shock, decreased cardiac output, hypotension, and so on. Concentrated urine (USG > 1.030 in dogs and >1.035 in cats) is an expected finding with prerenal azotemia. Renal azotemia can be due...