Biological Sciences
Efflux Pump
Efflux pumps are protein-based structures found in the cell membranes of bacteria and other organisms. They function to actively pump out toxic substances, including antibiotics and other drugs, from the cell, thereby contributing to antibiotic resistance. Efflux pumps play a crucial role in the defense mechanisms of bacteria and are a significant challenge in the treatment of bacterial infections.
Written by Perlego with AI-assistance
Related key terms
1 of 5
9 Key excerpts on "Efflux Pump"
- eBook - ePub
- Prashant Kesharwani, Sidharth Chopra, Arunava Dasgupta(Authors)
- 2020(Publication Date)
- Academic Press(Publisher)
Chapter 10Importance of Efflux Pumps in subjugating antibiotic resistance
Taru SinghaSajad Ahmad Dara , bShukla DasaShafiul Haqueba Department of Microbiology, University College of Medical Sciences (University of Delhi) and GTB Hospital, Delhi, Indiab Research and Scientific Studies Unit, College of Nursing and Allied Health Sciences, Jazan University, Jazan, Saudi ArabiaAbstract
Antibiotic resistance is defined as a condition that assists any disease-causing organism to resist antibiotics of different class with distinct structure and function directed for its elimination, thereby enabling the survival of the microorganism. Multiple resistance determinants play a major mechanism of bacterial resistance including multidrug Efflux Pumps. Different types of Efflux Pump mechanisms, such as single drug or multidrug-specific, are the significant determinants of resistance, either intrinsic or acquired, to the respective antibiotics. This has resulted in the development of Efflux Pump inhibitors (EPIs). By understanding the working mechanism of the Efflux Pump, various antibacterial agents known as efflux reversals can be described as EPIs, membrane permeabilizers, blockers, energy poisons, etc. Over the last few years a lot of effort was exerted to identify the new and unique EPIs; however, none was found suitable. - Dibyajit Lahiri, Moupriya Nag, Rina Rani Ray, Sougata Ghosh, Dibyajit Lahiri, Moupriya Nag, Rina Rani Ray, Sougata Ghosh(Authors)
- 2023(Publication Date)
- CRC Press(Publisher)
Bacterial Efflux Pumps diligently transport several antibiotics out of the cell and are contributors to the intrinsic resistance of Gram-negative bacteria to many of the drugs that are used to treat Gram-positive bacterial infections. Over expression of Efflux Pumps can also give high resistance to useful antibiotics which were previously effective. They can be specific for a single substrate (Tet pumps) or can transport a wide range of structurally diverse substrates and are known as MDR Efflux Pumps (Piddock, 2006). There are five main superfamilies of Efflux Pumps associated with MDR according to their composition, energy source, number of transmembrane spanning regions and substrates (Figure 5.1): Figure 5.1 Schematics diagram showing the main five superfamilies of Efflux Pumps fund in bacteria and their energy-coupling mechanisms. OM, outer membrane; IM, inner membrane. The multi-drug and toxic compound extrusion (MATE) family: proteins that are predicted to have 12 alpha-helical transmembrane regions (Kuroda and Tsuchiya, 2009), such as MepA. The small multidrug resistance (SMR) family: composed of four transmembrane alpha-helices of approximately 100–140 amino acids in length, for example, Smr (Jack et al., 2001 ; Bay et al., 2017) The major facilitator superfamily (MFS): proteins that transport a broad spectrum of ions and solutes across membranes via facilitated diffusion, symport, or antiport, such as NorA, NorB, NorC, MdeA, SdrM, LmrS (Pao et al., 1998, Yan, 2015) The ATP-binding cassette (ABC) superfamily (Lubelski et al., 2007): transporters that are remarkably conserved in terms of the primary sequence and the organization of the domains or subunits- Eric J. Toone(Author)
- 2011(Publication Date)
- Wiley(Publisher)
Chapter 3 Efflux Pumps of the Resistance–Nodulation–Division Family: A Perspective of their Structure, Function, and Regulation in Gram-Negative Bacteria By Mathew D.Routh Molecular, Cellular and Developmental Biology Interdepartmental Graduate Program, Iowa State University, Ames, Iowa Yaramah Zalucki Chih-Chia Su Department of Microbiology and Immunology, Emory University School of Medicine, Atlanta, Georgia Feng Long Molecular, Cellular and Developmental Biology Interdepartmental Graduate Program, Iowa State University, Ames, Iowa Qijing Zhang Department of Veterinary Microbiology and Preventive Medicine, College of Veterinary Medicine, Iowa State University, Ames, Iowa William M.Shafer Department of Microbiology and Immunology, Emory University School of Medicine, Atlanta, Georgia, and Laboratories of Microbial Pathogenesis, VA Medical Center, Decatur Georgia, and Edward W.Yu Molecular, Cellular and Developmental Biology Interdepartmental Graduate Program, Department of Chemistry, Department of Physics and Astronomy, and Department of Biochemistry, Biophysics and Molecular Biology, Iowa State University, Ames, Iowa I. Introduction With the initial discovery of penicillin and the ensuing mass production of antibiotics in the 1940s, infectious bacteria quickly adapted and developed resistance to the deleterious molecules. In fact, a report published in 1947 found that of 100 Staphylococcus infections tested, 38 were classified as highly resistant to penicillin (1). The initial resistance was associated primarily with individual enzymes inactivating specific antibiotics, such as β-lactamases on penicillin. As novel antibiotics were implemented to combat resistant pathogens, selective pressure led to fundamentally new methods of drug resistance. Currently, there are roughly three major mechanisms utilized by bacteria to evade the toxic effects of biocidal agents- eBook - ePub
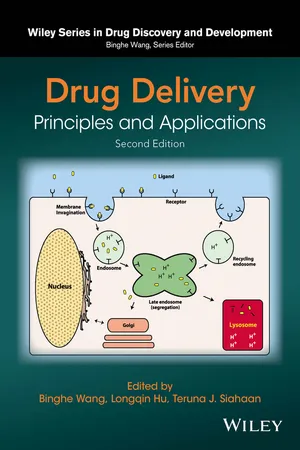
Drug Delivery
Principles and Applications
- Binghe Wang, Longqin Hu, Teruna J. Siahaan(Authors)
- 2016(Publication Date)
- Wiley(Publisher)
5 THE ROLE OF TRANSPORTERS IN DRUG DELIVERY AND EXCRETION Marilyn E. Morris and Xiaowen GuanDepartment of Pharmaceutical Sciences, School of Pharmacy and Pharmaceutical Sciences, University at Buffalo, State University of New York, Buffalo, NY, USA5.1 INTRODUCTION
Therapeutic agents or other xenobiotic compounds can exert their pharmacological or toxicological activities only when sufficient concentrations of the compounds are present at the site of action and upon binding to the targeted receptors or enzymes. Therefore, the ability of drug molecules to cross biological membranes represents an important determinant of drug absorption, distribution, metabolism, elimination, and, ultimately, their therapeutic or toxic effects. It is known that the complex biological membrane system is not pure lipid bilayers, but lipid bilayers embedded with numerous proteins, including transporters. The fundamental role of transporters is to maintain the cellular homeostasis and to provide physiological function for movement of endogenous substances, such as amino acids, glucose, and hormones; however, many of these transporters are also involved in transporting therapeutic agents. Thus, for a large number of drug molecules, their ability to pass through biological membranes is not only solely determined by their physiochemical parameters such as lipophilicity but also governed by drug transporter activities.Drug transporters are classified into two families: the ABC (ATP-binding cassette) and SLC (solute carrier) families. As the name implies, ABC transporters are primary active transporters that utilize ATP as the source of energy. ABC transporters are efflux transporters that transport substrates out of the cell. Members of ABC family that are important in drug excretion include P-glycoprotein (P-gp), multidrug resistance-associated proteins (MRPs), and breast cancer resistant protein (BCRP). In addition, these ABC transporters are also known to transport a number of clinically important anticancer agents, thereby limiting intracellular accumulation of these drugs and resulting in inefficient tumor cell killing, a phenomenon known as multidrug resistance (MDR) that is attributed to overexpression of these transporters on tumor cells [1–4]. In contrast SLC transporter families are secondary active transporters that use the concentration gradient of a cosubstrate such as protons or sodium ions to drive their transport. SLC transporters are mostly influx transporters that transport substrates from the extracellular lumen into the cell; exceptions to this are monocarboxylate transporters (MCTs) 1 and 4 and multidrug and toxin extrusion (MATE) transporters that can function as efflux transporters. - eBook - ePub
Antibiotics
Targets, Mechanisms and Resistance
- Claudio O. Gualerzi, Letizia Brandi, Attilio Fabbretti, Cynthia L. Pon, Claudio O. Gualerzi, Letizia Brandi, Attilio Fabbretti, Cynthia L. Pon(Authors)
- 2013(Publication Date)
- Wiley-VCH(Publisher)
H. influenzae strains, parental strain and isogenic derivative lacking AcrB. Four key points are discussed: the location of antibiotic target (periplasm vs cytoplasm), irreversible binding on bacterial target, self-promoted uptake, and ion trapping. These key parameters strongly contribute to the antibacterial behavior of the molecule and favor their intracellular concentration [162]. These respective properties are directly associated, again, with pharmacophoric groups and also with the targeted bacterium. Alternate ways can be also proposed by using blockers of OM channel (e.g., TolC, OprM), but at this moment, no molecules have been described. For other ways, poisoning the transport energy or altering the functional assembly of the Efflux Pump, no results supporting a possible clinical way have been reported [103].The increased level of overall understanding of drug influx and efflux is mandatory to develop new strategies and novel drug discovery efforts against MDR gram-negative bacteria. Molecules changing the barrier properties of the OM lipid bilayer itself or modulating the activity of Efflux Pumps can have a direct impact not only on gram-negative bacteria susceptibility but also on the fitness of bacteria. Consequently, their use favors a bacterial adaptation and the emergence of a new resistant generation. Whatever the selected ways, increasing the penetration or blocking the efflux activity, we must anticipate being ready to face the emergence of new resistances against the adjuvant/escort molecule used in combination. Appropriate investigations, from functional pharmacochemical to bacteriological-genetic, must be carried out to determine the best efficient combination, the targeted bacterium and the possible and future associated risk (selection and dissemination of resistant mutants). - W.N. Konings, H.R. Kaback, J.S. Lolkema(Authors)
- 1996(Publication Date)
- North Holland(Publisher)
Third, the present knowledge of the molecu- lar mechanisms involved in drug transport processes will be discussed. It is hoped that this brief introduction will encourage the reader to delve more deeply into the wealth of scientific material which follows. 2. Classification of prokaryotic drug extrusion systems Currently, over 30 drug transporters have been discovered in prokaryotes. On the basis of bioenergetic and structural criteria, these transport systems can be divided into: (i) secondary drug transporters, and (ii) ATP-binding cassette (ABC)-type drug transporters. The secondary drug transporters are single membrane proteins which mediate the extrusion of drugs in a coupled exchange with protons (or sodium) ions [21 ]. In this exchange process, the ion motive force can drive the efflux of drugs against a concentration gradient. On the basis of similarities in size and secondary structure, the secondary drug transporters can be divided into two subgroups. The members of these subgroups are referred to as TEXANs (Toxin EXtruding ANtiporters) and Mini TEXANs [22]. TEXANs are about 45-50 kDa with a hypothesized topology of 12-14 transmembrane ~-helical domains [23]. This subgroup includes all mem- bers of the drug resistance branch of the Major Facilitator superfamily of trans- porters [24], and some members of the Resistance-Nodulation-Division family of membrane proteins [25]. Mini TEXANs are functionally similar to TEXANs, but are much smaller (12-15 kDa) and form only 4 putative membrane spanning domains [26]. The ABC-type drug transporters belong to the ABC superfamily, the members of which contain a highly conserved ATP-binding cassette [27-30]. They utilize the energy of ATP hydrolysis to pump cytotoxic substrates out of the cell [31]. Typically, ABC transporters require the function of four protein domains [27,32]. Two of these domains are highly hydrophobic and each consist of 6 putative transmembrane segments.- eBook - PDF
- Varaprasad Bobbarala(Author)
- 2012(Publication Date)
- IntechOpen(Publisher)
However, under particular circumstances, the outer membrane barrier cannot be the whole explanation of the bacteria resistance to inhibitors (Nikaido 1996). In fact, the equilibration across the outer membrane is reached very quickly, in the part of the surface-to-volume ratio that is very large to compare with bacterial cell size. Thus, the periplasmic concentration of many antibiotics may achieve 50% of their external value (Nikaido, 1989). In the literature, numerous plasmid and chromosome-encoded efflux systems, both agent- or class-specific and multidrug have been performed in a various of microorganisms where they are the major determinant in the intrinsic resistance of the bacteria to action of dyes, detergents and different classes of antibiotic including β -lactams (Nikaido, 1989; Nikaido, 1994; Markham & Neyfakh, 2001; Butaye et al., 2003). Bacterial Efflux Pumps compose of five classes of systems including: the major facilitator superfamily (MF), the ATP-binding cassette family (ABC), the resistance-nodulation-division family (RND), the small multidrug resistance family (SMR), and the multidrug and toxic compound extrusion family (MATE) (Putman et al., 2000; Kumar & Schweizer, 2005; Poole & Lomovskaya, 2006). To drive antimicrobial agents efflux, the ABC family system hydrolyses ATP, whereas the MF family, the RND family and the MATE family function as secondary transporters, catalysing drug-ion antiport (H + or Na + ) (Poole, 2005). The RND family transporters are most commonly found in bacteria cells (Poole, 2001). In gram-negative bacteria this system operates as a part of a tripartite mechanism that includes: a membrane fusion protein that is associated with the cytoplasmic membrane, a transporter protein that export substrates throughout the inner membrane, and an outer membrane factor (OMF) that enables the passage of the substrate throughout the outer membrane (Poole, 2005). - eBook - PDF
- Richard G. Wax, Kim Lewis, Abigail A. Salyers, Harry Taber, Richard G. Wax, Kim Lewis, Abigail A. Salyers, Harry Taber(Authors)
- 2007(Publication Date)
- CRC Press(Publisher)
45 4 Multidrug Efflux Pumps: Structure, Mechanism, and Inhibition Olga Lomovskaya, Helen I. Zgurskaya, Keith A. Bostian, and Kim Lewis CONTENTS MDRs in Clinically Relevant Drug Resistance .................................................... 46 Antiinfective Drug Discovery and Efflux Pump Inhibitors ................................. 53 Perspectives for Developing MDR Inhibitors ....................................................... 56 Natural MDR Inhibitors ....................................................................................... 59 Concluding Remarks ............................................................................................ 61 References ............................................................................................................. 61 The world of antibiotic drug discovery and development is driven by the necessity to overcome antibiotic resistance in common Gram-positive and Gram-negative pathogens. However, the lack of Gram-negative activity among both recently approved antibiotics and compounds in the developmental pipeline is a general trend. It is despite the fact that the plethora of covered drug targets is well conserved in both Gram-positive and Gram-negative bacteria. Multidrug resistance (MDR) Efflux Pumps play a prominent and proven role in Gram-negative intrinsic resistance. More-over, these pumps also play a significant role in acquired clinical resistance. Together, these considerations make Efflux Pumps attractive targets for inhibition in that the resultant Efflux Pump inhibitor (EPI)/antibiotic combination drug should exhibit increased potency, enhanced spectrum of activity, and reduced propensity for acquired resistance. To date, at least one class of broad-spectrum EPI has been extensively characterized . While these efforts indicated a significant potential for developing small molecule inhibitors against Efflux Pumps, they did not result in a clinically useful compound. - eBook - ePub
Ocular Transporters and Receptors
Their Role in Drug Delivery
- Ashim K Mitra(Author)
- 2013(Publication Date)
- Woodhead Publishing(Publisher)
0’+ ), the organic anion transporting polypeptide family and sodium-dependent multivitamin transporter. In this chapter, the biology of Efflux Pumps and influx transporters with special emphasis on membrane topology, structural conformations, tissue localization and distribution, transport mechanisms, genomic properties and some important mutation sites are discussed in detail.Key words Influx transporters Efflux Pumps biology transmembrane domains membrane topology tissue localization and distribution2.1 Introduction
The integrity of cellular lipid bilayer membranes is critically important for the functioning of the cells. Diffusion of polar molecules across the lipid bilayer is limited, so transporters have evolved to transport vital substances (anions, cations, vitamins, sugars, nucleosides, amino acids, peptides etc.) into the cells and to eliminate toxic materials out of the cells, so maintaining cellular homeostasis. Transporters are membrane/cytosolic proteins that are an integral part of all organisms. These transporters, in humans, play a significant role in the process of drug absorption, distribution, metabolism and elimination (ADME). In essence with their central role of cellular viability, of the 2000 genes in the human genome, about seven of the genes code for transporters or transporter-related proteins [1 ]. There are 400 membrane transporters in two superfamilies and many of these transporters have been identified, cloned and characterized with specific tissue localization profiles [2 ]. From the pharmacological point of view, the transporters are classified into two major superfamilies, i.e. ABC (ATP-binding cassette) and SLC (solute carrier) transporters. ABC transporters act by ATP hydrolysis to actively pump their substrates across the lipid bilayer. These proteins are encoded by 49 genes and are grouped into seven subclasses (ABCA to ABCG) [3 ]. The best documented transporter in the ABC superfamily is the P-glycoprotein (P-gp) encoded by the MDR1 gene and it is responsible for the efflux of several drug molecules. The SLC super family comprises 43 families and contributes to drug absorption [4 ]. There are many well-known SLC transporters including serotonin (SLC6A4 ) and dopamine (SLC6A3 ) transporters. Apart from carrying nutrients or extruding cellular waste/toxins, the broad role of membrane transporters is in drug absorption, distribution and elimination. Further, the role of membrane transporters in drug–drug interactions and multidrug resistance has been well documented. In addition to drug delivery, some of the transporters also serve as a protective barrier for particular organs or cell types. For example, P-gp in the blood–brain barrier or blood–retinal barrier protects the brain and eyes, respectively, from toxic insults by efflux of a variety of structurally diverse compounds. ABC efflux transporters also function in conjunction with drug metabolizing enzymes to eliminate drugs and their metabolites. Molecular cloning of transporter genes delineates the involvement of multiple genes encoding subtypes with similar function with different tissue distribution and specificity towards drugs. Studying these subtypes (e.g. glucose transporters, GLUT 1–4) can unravel the complexities of the structure–activity relationship for drug transport and may allow modulation of transporter activity when needed. Transporters exist in the form of multiple alleles, some of which encode proteins with functional defects resulting in defective drug binding or transport. Although the importance of drug transporters in the process of ADME and drug-drug interactions is well recognized, our knowledge on the biology/physiology of transporters is still emerging. There is a large body of information available in the review published earlier by Sadee et al. [5
Index pages curate the most relevant extracts from our library of academic textbooks. They’ve been created using an in-house natural language model (NLM), each adding context and meaning to key research topics.